Pedia 2017 2018
A 3-day-old, full-term baby boy is brought into the emergency department because of feeding intolerance and bilious vomiting. X-rays films show multiple dilated loops of small bowel and a "ground glass" appearance in the lower abdomen. The mother has cystic fibrosis. Which of the following diagnostic tests would also have therapeutic value?
Barium enema
Gastrografin enema
Endoscopic retrograde chokngiopancreatogram (ERCP)
Full thickness rectal biopsy
Colonoscopy
A 3-year-old boy is brought to the office by his Caucasian mother because his speech is difficult to understand. He is a very slow learner, is unusually calm, stays to himself, doesn't hug his parents, prefers to play by himself, speaks in mumbles, and repetitively tries to make towers with cubes. He becomes very aggressive if he is stopped from his activities. He was born at term from an uncomplicated pregnancy and delivery, and his physical growth has been normal. His brother used to be aggressive as a child, and was diagnosed with attention deficit hyperactivity disorder. In the office, the patient is sitting quietly and trying to make towers with cubes. He seems to be oblivious of his environment. On calling his name thrice, he turns towards you once and then resumes playing with the cubes. What do you tell his mother?
His diagnosis is Asperger syndrome
This could be autism and would benefit from antipsychotics
He has autism and will need special behavioral and educational programs
He has attention deficit hyperactivity disorder and would benefit from methylphenidate
He has hearing problems and he needs ear, nose and throat evaluation
The parents of a 2-month-old baby boy are concerned about his risk of coronary artery disease because of the recent death of his 40- year-old maternal uncle from a myocardial infarction. Which of the following is the most appropriate management in this situation?
Screen the parents for total cholesterol
Recommend yearly ECGs for the patient
Counsel the parents regarding appropriate dietary practices for a 2-month-old infant and test him for total cholesterol at 6 months of age
Initiate lipid-lowering agents
Reduce the infant’s dietary fat to less than 30% of his calories by giving him skim milk
A one-week-old infant is admitted to the neonatal intensive care unit due to vomiting, abdominal distension, and poor feeding. His vomitus is bile-stained. There is frank blood in his stools. He has been formula- fed since birth. Physical examination shows diminished bowel sounds. Abdominal x-rays reveal dilated loops of bowel with intramural air Laboratory studies show elevated WBCs. What is the most likely diagnosis?
Food poisoning
Hirschsprung's disease
Duodenal atresia
Pyloric stenosis
Necrotizing enterocolitis
A 2-year-old child is referred to hospital by the GP after his third visit that week; he now has a rash and the GP is worried he has meningitis. He has had a fever for 5 days up to 39.5°C or above every day and is not eating or drinking well. On examination, he has a temperature of 38.5°C, heart rate of 150, and respiratory rate of 30 and is miserable. He has a blanching macular rash on his torso, swollen hands and feet, red eyes, red cracked lips, large tonsils with no pus, and a left-sided 2 cm× 3 cm cervical lymph node which is mobile. There is no photophobia or neck stiffness. His chest is clear with normal heart sounds and his abdomen is soft with a palpable liver edge. You note his BCG scar is inflamed. What is the most likely diagnosis?
Kawasaki’s disease
Viral tonsillitis
Meningitis
Bacterial tonsillitis
Hand, foot and mouth disease

The 1-year-old boy in the photograph below, who recently had a circumcision, requires an additional operation on his genitalia that will probably eliminate his risk of which of the following?
Torsion of testes
Epididymitis
Urinary tract infection
Testicular malignancy
Decreased sperm count
A previously healthy 7-year-old girl comes to the office with complaints of episodic abdominal pain over the past several months. The pain is periumbilical and sharp but does not wake her from sleep or interfere with play. She has no fever, joint complaints, or constipation or diarrhea. Growth and development have been normal. The physical examination is within normal limits. Which of the following is the most likely diagnosis?
Acute appendicitis
Acute cholecystitis
Crohn disease
Functional abdominal pain
Irritable bowel syndrome
A previously healthy 7-year-old child suddenly complains of a headache and falls to the floor. When examined in the emergency room (ER), he is lethargic and has a left central facial weakness and left hemiparesis with conjugate ocular deviation to the right. Which of the following is the most likely diagnosis?
Acute infantile hemiplegia
Acute subdural hematoma
Supratentorial tumor
Hemiplegic migraine
Todd paralysis
A 2-hour-old male neonate has developed worsening cyanosis over the past few minutes. The infant was vaginally delivered (assisted with forceps) at full term and weighed 4.1 kg (9 lb). The Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Oxygen is administered by mask but does not relieve the cyanosis. Further examination reveals tachypnea, subcostal retractions, a normal first heart sound, a single and loud second heart sound (S2), and no murmur. Which of the following is the most likely cause of the infant's cyanosis?
Patent ductus arteriosus
Coarctation of the aorta
Atrial septaI defect
Transposition of the great vessels
Ventricular septal defect
A 20-year-old female is brought to the Emergency Room by her college roommate who states that the patient vomited all night. The patient complains of a sore throat and says she has not eaten for the last two days. She admits to a "sugar problem" and quit taking her medication because she has not been eating. Examination reveals an ill-appearing woman. Her temperature is 37.9 C (100.2 F), blood pressure is 118/78 mm Hg, pulse is 160/min, and respirations are 30/min. The patient's lips and mucous membranes are dry. There is a fruity odor noted to the patient's breath. The lung and cardiac examination are unremarkable except for mild tachypnea and tachycardia. Laboratory analysis shows: Sodium 130 mEq/L, Potassium 6.1 mEq/L, Chloride 100 mEq/L, Bicarbonate 8 mEq/L, Urea nitrogen 10 mg/dL, Creatinine 1.0 mg/dL, Glucose 680 mg/dL, pH 7.15, pCO2: 30 mm Hg, pO2: 85 mm Hg, Urinalysis is positive for ketones. Which of the following is the most appropriate initial step in management?
Mannitol
Immediate intubation
Intravenous insulin
Intramuscular ceftriaxone
IV fluid bolus with normal saline and potassium
A 3-month-old baby is brought to accident and emergency because he has been vomiting and having diarrhoea for the past month. His mother breastfed him until he was 8 weeks old and he is now taking formula milk, 4–5 oz every 4 hours. On examination he is alert but fussy and looks thin. He has eczema on his face, neck and torso and the mother says this is new. The abdomen is soft, the genitalia are normal with a significant nappy rash and the anal margin is erythematous. You plot his growth in his red book and find that he was born on the 50th centile and was following that but now he is on the 25th centile for weight. What is the most likely diagnosis?
Hyper IgE syndrome
Lactose intolerance
Wiskott–Aldrich syndrome
Gastroenteritis
Cow’s milk protein intolerance
A mentally retarded 10-year-old boy presents with arthritis, nephrolithiasis, and progressive renal failure. Since his first years of life, he manifested peculiar neurologic abnormalities consisting of self-mutilative biting of the lips and fingers, choreoathetosis, and spasticity. Two male relatives on his mother's side presented with a similar condition and died in their teens. Which of the following is the most likely diagnosis?
Huntington disease
Chronic lead intoxication
Gout
Lesch-Nyhan syndrome
Fragile-X syndrome
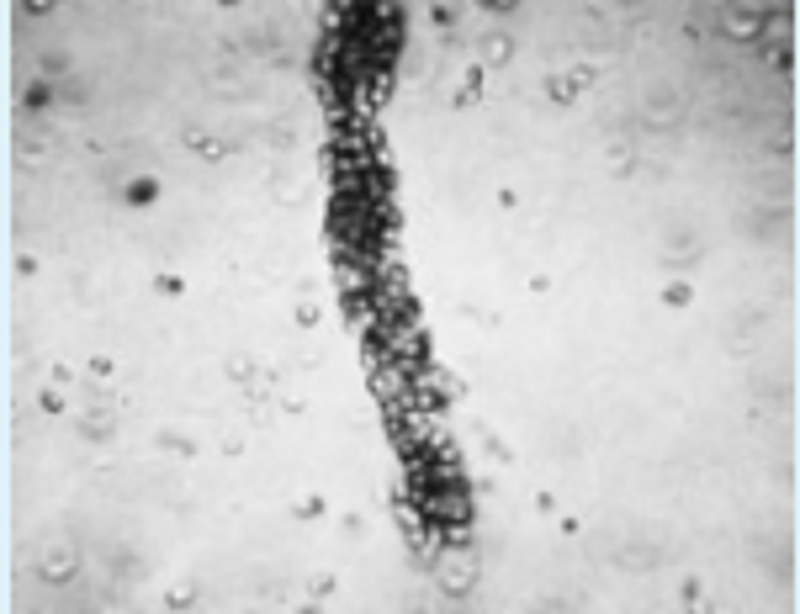
The photomicrograph below is of a urine specimen from a 15-year-old girl. She has had intermittent fever, malaise, and weight loss over the previous several months. Recently she has developed swollen hands, wrists, and ankles, the pain of which seems out of proportion to the clinical findings. She also complains of cold extremities and has some ulceration of her distal digits. Which of the following laboratory tests is most likely to assist in the diagnosis of this condition?
A urine culture
Throat culture for group A β-hemolytic streptococcus
Erythrocyte sedimentation rate
Antibodies to nDNA and Sm nuclear antigens
Simultaneously acquired urine and serum bicarbonate levels
A 7 -year-old boy is brought to the office by his mother due to nocturnal enuresis. He has been wetting his bed at night for the past two years. He is otherwise healthy and has no psychological or behavioral problems. His mother is desperately asking for your help because she has tried alarms and bladder training, all to no success. What is the most appropriate next step in the management of this patient?
Clonidine
Haloperidol
Desmopressin
Insulin
Prazosin
You see an 18-year-old boy who is the first child of his African parents and was born in Kenya before moving to the UK 1 year ago. He has white skin and pink irises. He was diagnosed with oculocutaneous albinism at birth. He has difficulty with his sight but has recently developed a skin lesion on his face. His mother has brought him to his GP as it has recently started to increase in size. On examination you note is an elevated, 3 cm diameter lump on the left of his nose. It has irregular edges, is firm and immobile and pigmented in areas. What is the likely diagnosis?
Benign naevus
Wart
Scar from a healing wound
Abscess
Malignant tumour
A 15-year-old boy attends his GP with a week of cough productive of yellow sputum, fever to 39°C and chest pain on the right side of the chest on coughing. There is no history of foreign travel or unwell contacts. On examination there is reduced air entry in the right lower zone with crepitations and bronchial breathing. You diagnose a right-sided chest infection. What is the most likely causative organism?
Staphylococcus aureus
Chlamydophila pneumoniae (Chlamydia pneumoniae)
Streptococcus pneumoniae
Mycoplasma pneumoniae
Mycobacterium tuberculosis
A 16-year-old boy presents to the emergency center with a 2-day history of an abscess with spreading cellulitis. While in the emergency center, he develops a high fever, hypotension, and vomiting with diarrhea. On examination you note a diffuse erythematous macular rash, injected conjunctiva and oral mucosa, and a strawberry tongue. He is not as alert as when he first arrived. This rapidly progressive symptom constellation is likely caused by which of the following disease processes?
Kawasaki disease
Neurotoxin-secreting Clostridium tetani
α-Toxin–secreting Clostridium perfringens
TSST-1–secreting S aureus
Shiga toxin–secreting Escherichia coli
A 5-year-old boy is brought to the physician because of a malodorous discharge coming from his right nostril. His parents report that the child developed frequent sneezing and mucus discharge for one week. They thought it was a common cold. The child is afebrile and in apparent good health. There is no history of allergic diseases or recurrent infections. Examination reveals obstruction of the right nasal fossa with associated purulent discharge from the right nostril. Which of the following is the most likely diagnosis?
Juvenile angiofibroma
Nasal foreign body
Nasal polyp
Allergic rhinitis
Rhinitis medicamentosa
A 2-year-old boy is brought to your clinic because he has a nighttime cough. According to his mother, several times over the past few months he has awakened with a barking, nonproductive cough that improves by the next morning. She denies fever and rhinorrhea with the episodes. Evaluation of his lungs yields normal results. Of the following, the clinical feature that is MOST suggestive of spasmodic croup rather than recurrent laryngotracheobronchitis in this boy is
Nonproductive nature of the cough
Lack of rhinorrhea and fever
Normal findings on physical examination
Age of the patient
Barking nature of the cough
A 12-year-old boy is brought to the office by his mother due to a two-week history of generalized edema which is gradually progressing. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/80 mmHg, pulse is 85/min, respirations are 18/min, and temperature is 36.7C (98F). The laboratory findings are as follows: Serum sodium 140 mEq/L, Serum potassium 3.7 mEq/L, Serum albumin 2.1 g/dl, Serum globulin 6.0 g/dl, Serum creatinine 1.0 mg/dl. Urinalysis reveals proteinuria 3+. What is the best next step in the management of this patient?
Renal biopsy
Prednisone
Scintigraphy
Intravenous pyelography (IVP)
Prednisone and cyclophosphamide
A 17-year-old boy comes to medical attention because of recurrent sinusitis and pneumonia, and persistent watery diarrhea due to Giardia lamblia. His parents and a sister are in excellent health. Physical examination reveals enlarged lymph nodes in cervical, axillary and inguinal regions. A lymph node biopsy shows hyperplastic follicles with an absence of plasma cells. Laboratory investigations show: Hematocrit44%, Leukocyte count9, 800/mm3, Neutrophils55%, Lymphocytes30%, Monocytes5%, CD4 T-cell count1000 cells/mm3, Proteins, serum6.2 g/dL, Albumin5.0 g/dL, Globulin1.2 g/dL. Additional studies demonstrate severely depressed levels of serum IgG, with slightly below-normal levels of IgM and IgA. Which of the following is the most likely diagnosis?
X-linked agammaglobulinemia of Bruton
Hodgkin disease
Common variable immunodeficiency
Isolated IgA deficiency
Acquired immunodeficiency syndrome (AIDS)
A 10-year-old boy presents with recurrent mouth ulcers, abdominal pain, distension and frequent episodes of diarrhoea with mucus. He has been losing weight. On examination he is slim and plotting his growth shows a fall in weight from the 50th centile to below the 9th. His abdomen is soft with generalized discomfort on deep palpation but no masses are present. What is the most likely diagnosis?
NEC
Crohn’s disease
Coeliac disease
Ulcerative colitis
Gastroenteritis
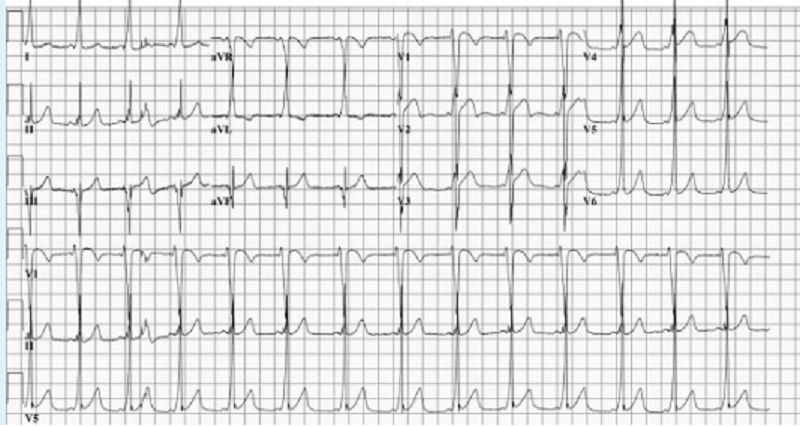
A 4-year-old girl is brought to the pediatrician’s office. Her father reports that she suddenly became pale and stopped running while he had been playfully chasing her and her pet Chihuahua. After 30 minutes, she was no longer pale and wanted to resume the game. She has never had a previous episode and has never been cyanotic. Her physical examination was normal, as were her chest x-ray and echocardiogram. An ECG showed the pattern seen on the next page, which indicates which of the following?
Paroxysmal supraventricular tachycardia
Excessive stress during play
Stokes-Adams pattern
Wolff-Parkinson-White syndrome
Paroxysmal ventricular tachycardia
An 18-month-old boy presented to the GP with a history of eating soil. He had been in the garden this afternoon as his mother put the washing out. She found him eating the soil and took him straight inside. On examination, he is well and alert but has pale conjunctivae. He is not tachycardic or tachypnoeic. His diet consists of predominantly of breast milk. What is the most likely result of his haemoglobin and haematinics?
Hb 7 g/dL, MCV 70 fl, ferritin normal, iron normal, vitamin B12 and folate normal
Hb 6.8 g/dL, MCV 65 fl, ferritin normal, iron low, vitamin B12 and folate normal
Hb 10 g/dL, MCV 80 fl, ferritin normal, iron normal, vitamin B12 and folate normal
Hb 6.5 g/dL, MCV 100 fl, ferritin normal, iron normal, vitamin B12 and folate low
Hb 5.5 g/dL, MCV 55 fl, ferritin low, iron low, vitamin B12 and folate normal
A term male infant is found to be cyanotic shortly after birth and requires endotracheal intubation. On physical examination, his blood pressure is 68/34 mm Hg (equal in all four extremities), pulse is 180/min, and respirations are 32/min. His precordium is dynamic, has a grade III systolic murmur, and a single S2. Chest radiography shows a normal heart size and increased pulmonary vascular markings. An arterial blood gas on an FiO2 of 100% shows pH 7.34; PaCO2: 47 mm Hg; PaO2: 46 mm Hg. Which of the following diagnoses is most consistent with these findings?
Tetralogy of Fallot
Patent ductus arteriosus
Total anomalous pulmonary venous return
Atrial septal defect
Hypoplastic left heart syndrome
A 7-year-old boy presents with a rash. His mother states that he was well until 3 days ago when he developed fever and malaise. The next day, the rash started as papules on the trunk, which rapidly changed to vesicles. The lesions have spread all over the body. On physical examination, he has no fever and seems well. You note numerous vesicles all over the body, some of which have crusted over. Which of the following is the most likely diagnosis?
Chicken pox
Staphylococcal scalded skin syndrome
Kawasaki disease
Rubella
Measles
A 7-year-old boy is brought to the physician because of recurrent headaches. The child feels nauseated before and during each attack, and derives some relief from lying down in a dark room. Noises, bright light, and fatigue seem to trigger the episodes. The child frequently complains of headaches at school, and his mother has been occasionally compelled to take him home. The mother is worried about the possibility of a serious illness. She reports that the child's father has similar headaches. The child's growth is normal, and a neurologic examination fails to reveal any abnormality. Which of the following is the most likely diagnosis?
Tension headache
Conduct disorder
Cluster headache
Migraine
Brain tumor
A 9-year-old male is brought to the emergency department with respiratory disease after being stung by a bee. He requires resuscitation with epinephrine injection. On discharge, which of the following recommendations to the boy's mother is most appropriate?
Provide epinephrine to carry with him
Do not allow him to play outside
Use insect repellants
Give prophylactic antihistamine agents daily
Wear colorful clothes while outside
A 1-month-old infant is brought to the office for a routine neonatal visit. His prenatal and birth histories are unremarkable. His vital signs are normal. Examination reveals a harsh, loud holosystolic murmur over the left, lower sternal border. Palpation reveals a thrill over the precordial region. There is no cyanosis, and pulmonary auscultation reveals no rales. Chest radiograph reveals a heart of normal size and a slight increase in pulmonary vascularity. EKG is normal. Which of the following is the most appropriate course of action?
PGE 1 administration
Reassurance
Surgical repair
Oxygen administration
Digoxin and diuretic therapy
You are called to evaluate a male infant at 50 hours of age because he has not voided. He was born at term and has breastfed poorly, but has passed stool. He appears uncomfortable on physical examination, with a large abdomen and seemingly palpable bladder. There is no respiratory distress. The external genitalia are normal, and both testes descended. Of the following, the MOST appropriate initial step in this infant's evaluation is
Renal ultrasonography
Passing of a urinary catheter
Consultation with an urologist
Intravenous pyelography
Nuclear renal scan
A mother brings her 4-year-old son to see you. She seems to be very concerned about her child's bedwetting. As you explore the history, the mother tells you that she started his toilet training when he was 2 years old. The child responded to his mother's efforts and slowly was able to reduce the frequency of bedwetting. However, he did not completely succeed and still occasionally wets his bed. She has become so concerned that she demands you to order tests and prescribe some drugs to resolve the problem. What is your best next step in the management of this boy?
Do a KUB and then check for vesica-ureteric reflex.
Do urinalysis followed by culture and microscopy.
Start desmopressin for incontinence and antibiotics for the child's urinary tract infection
Immediately do an ultrasonogram, intravenous pyelogram and cystometrogram to establish a baseline level of fun
Reassure the mother that everything is normal and it will resolve with age
A 2-week-old baby girl is brought to the clinic for the evaluation of vaginal discharge. Her mother has noticed a cloudy white vaginal discharge mixed with blood since yesterday. She was born by normal vaginal delivery at term, and no congenital anomalies were noted at birth. Physical examination reveals a blood-stained, odorless vaginal discharge. Her vital signs are stable. What is the most appropriate next step in the management of this patient?
Treatment for Trichomonas vaginalis
Treatment for HSV-2
Treatment for Chlamydia
Reassurance
Rule out vaginal cancer
Within 8 hours after birth, an infant has "excessive salivation." Physical examination reveals that she has an imperforate anus, with a small fistula to the vagina. A small, soft nasogastric tube is inserted, and the infant is taken to x-ray. The film shows the tube coiled back on itself in the upper chest, and a normal gas pattern in the gastrointestinal tract. There are no apparent abnormalities of the radius or the vertebral bodies. Which of the following is the most appropriate next step in management?
Surgical repair of esophageal atresia
Diverting colostomy
Barium swallow
Placement of a gastrostomy tube
Renal sonogram and echocardiogram
A 5-week-old infant is brought to the clinic for a 4-week history of noisy breathing that has not improved. She has otherwise been healthy except for a current upper respiratory infection for the past 4 days, which according to the parents, has worsened the noisy breathing. On examination, she has inspiratory stridor. The noisy breathing improves when the infant is asleep. Which of the following is the most likely diagnosis?
Laryngomalacia
Bronchoalveolar carcinoma
Tuberculosis
Bacterial pneumonia
Foreign object obstruction
A 17-year-old teenage girl presents to your office after having problems during sex with her boyfriend. She also states that she has been developing facial hair, which she has constantly been removing. She started her menstruations at the age of 13 and her cycles have always been regular. On examination she is obese but appears a little masculine and has an enlarged clitoris. Initial lab values are as follows: Serum LH 20 IU/L, Serum FSH 10 IU/L, 17 -hydroxyprogesterone 600ng/ml (Normal is 15ng/ml), Serum testosterone Normal, Serum DHEA 4.0ng/ml (Normal is 4.2ng/ml). What is the most likely diagnosis?
Adrenal carcinoma
Polycystic ovarian disease
Cushing's syndrome
Cushing's disease
Congenital adrenal hyperplasia
A 30 weeks' gestation infant weighing 1,500 g experiences respiratory distress that requires assisted ventilation in the first 4 hours after birth. Some tachypnea with mild subcostal and intercostal retractions is evident on physical examination. Current ventilator parameters are: positive end-expiratory pressure of 4 cm H2O, peak inspiratory pressure of 22 cm H2O, synchronized ventilator rate of 40 breaths/min, and fraction of inspired oxygen of 0.8 to maintain a Pao2 of 60 mm Hg. A chest radiograph reveals low lung volumes, diffuse microatelectasis, and dense ground-glass opacities. You order surfactant for intratracheal administration. Of the following, the MOST expected event in the 4 hours following surfactant administration is
Decreased pulmonary compliance
Pulmonary hemorrhage
Decreased oxygen requirement
Increased inspiratory pressure
Hypotension
A 10-year-old boy is brought by his parents to the emergency department for the evaluation of headaches, fever, chills, and a rash over his neck, chest, and axillae. The rash appeared today, and for the past two days the child was complaining of a sore throat. He has no history of allergies, and his immunizations are up-to-date. His blood pressure is 112/70 mmHg, pulse is 1 08/min, respirations are 20/min, and temperature is 38.3C (101 F). Examination reveals an erythematous rash with a sandpaper-like texture, and which blanches with pressure. There is submandibular tender lymphadenopathy, and the throat is erythematous with gray-white exudates. What is the most likely diagnosis?
Stevens-Johnson syndrome
Staphylococcal scalded skin syndrome
Scarlet fever
Kawasaki disease
Mononucleosis
A 15-year-old postmenarcheal girl presents with persistent right lower quadrant discomfort of 6 weeks' duration and a feeling of abdominal fullness. Her last menstrual period was 3 weeks ago. Results of a urine pregnancy test are negative, and urinalysis results are normal. Ultrasonography reveals a well-defined right ovarian cyst filled with multiple echoes. Of the following, the BEST next step for the management of this patient is
Repeat ultrasonography in 4 to 8 weeks
Oophorectomy
Therapy with combined oral contraceptives
Laparoscopic cyst aspiration
Measurement of serum tumor markers
An 8-year-old girl is brought to see you, having not opened her bowels in 8 days. She complains of hard painful stools and recurrent abdominal pain for the past 6 months but no vomiting. Her mother thinks that she is avoiding going to the toilet and reports that she has always been a bit irregular opening her bowels, averaging about twice a week. In her past medical history, she passed meconium on day 1 of life and has had no significant medical problems. On examination she is a well-looking, normally grown child. Her abdomen is soft with a palpable indentable mass in the left iliac fossa. The anus is normal, as are her lower limbs. What is the first step in management?
Encourage her to increase her fluid intake, dietary fibre and exercise
Refer for bowel disimpaction under anaesthesia
Introduce scheduled toileting with a positive reward scheme such as a star char
Start a stimulant laxative such as senna
Start polyethylene glycol with electrolytes such as Movicol
A 3-year-old African-American female is brought to the office due to a swelling in her abdomen. According to her parents, this swelling was first noted when she was 3 months old, and has been increasing in size over the past 6 months. It is more pronounced during crying and coughing. Examination reveals a soft swelling of the umbilical region that is 3 cm in diameter and covered by skin. It can be easily reduced through the fibrous ring at the umbilicus. The child is afebrile and in good health. What is the most likely diagnosis and best course of action for this patient?
Umbilical hernia, observe for spontaneous resolution
Umbilical hernia, refer to pediatric surgeon for operative management
Umbilical polyp, surgical excision
Gastroschisis, surgical management
Congenital omphalocele, refer to pediatric surgeon
A 10-year-old boy is brought to the paediatric outpatient department for a review of his height. He was found to be on the 0.4th centile and his mid-parental height is the 98th centile. He also has widely spaced nipples, wide carrying angle, hypogonadism, pulmonary stenosis and developmental delay. What is the most likely diagnosis?
Turner’s syndrome
Angelman’s syndrome
Prader–Willi syndrome
Noonan’s syndrome
Williams’s syndrome
A 3-year-old-boy ingests 40 of his older sister's chewable vitamin tablets, as well as 3 tablets of 250 mg of acetaminophen. The ingredients in the multivitamin tablets are as follows: Vitamin A 3000 IU, Thiamine 1 mg, Vitamin C 75 mg, Vitamin B6 1 mg, Vitamin D 400 IU, Iron 12 mg, Fluoride 1 mg. The child is brought to the emergency department in no acute distress. Which of the following complications may occur if appropriate therapy is not undertaken?
Hepatic failure from acetaminophen toxicity
Acute renal failure from vitamin D toxicity
Hepatic failure from iron toxicity
Increased intracranial pressure from vitamin A toxicity
Intestinal ischemia from fluoride toxicity
A 2-year-old child is brought to cardiology clinic due to a heart murmur heard by the GP after an examination when she was recently unwell. She was born at 40 weeks by normal vaginal delivery but was noted to have a cleft palate at birth. She was kept in hospital for establishment of feeding but during this time she had a seizure, noted later to be because her calcium was low. You hear a harsh, grade 3/6 pansystolic murmur, loudest at the left lower sternal edge, consistent with a ventral septal defect (VSD) as seen on echocardiogram. With this history and current examination finding, you wish to exclude DiGeorge’s syndrome. What is the best diagnostic test?
Identification of specific mutation
FISH (fluorescence in situ hybridization)
ELISA (enzyme-linked immunosorbent assay)
Karyotype
Geneticist review and diagnosis

Over the previous 2 to 3 weeks, a very active 13-year-old white boy is noted by his family to have developed deep pains in his leg that awaken him from sleep. The family brings him to your office with a complaint of a swelling over his distal leg, which he attributes to his being kicked while playing soccer about 1 week ago. He has had no fever, headaches, weakness, bruising, or other symptoms. A radiograph of the leg is shown below. Which of the following is the most likely explanation for his pain?
Growingpains
Leukemia
Bone fracture
Osteomyelitis
Osteosarcoma
A 14-year-old boy presents with sudden onset of pain and swelling of his right testicle. There was no history of trauma, he is not sexually active, and denies any history of penile discharge. On examination, the scrotum is swollen and tender. The cremasteric reflex is absent. A testicular flow scan shows a “cold spot” or absent flow to the affected side. Which of the following is the most likely cause?
Epididymitis
Inguinal hernia
Torsion of the appendix testis
Hydrocele
Testicular torsion
The mother of a 4-year-old child takes her daughter to a pediatrician because she is "scratching all the time." Physical examination demonstrates multiple areas of excoriation, which are worst on the shoulders, buttocks, and abdomen. In the areas where the scratching has occurred, scattered tiny red punctate lesions are also seen. Careful examination of the clothing reveals small, ovoid, grayish-white structures attached to threads on the seams. Which of the following is the most likely causative agent?
Trichophyton rubrum
Sarcoptes scabiei
Corynebacterium minutissimum
Ancylostoma braziliense
Pediculus humanus corporis
A 13-year-old patient with sickle-cell anemia presents with respiratory distress; she has an infiltrate on chest radiograph. The laboratory workup of the patient reveals the following: hemoglobin 5 g/dL; hematocrit 16%; white blood cell count 30,000/µL; and arterial blood (room air) pH 7.1, PO2: 35 mm Hg, and PaCO2: 28 mm Hg. These values indicate which of the following?
Acidemia, metabolic acidosis, respiratory alkalosis, and hypoxia
Primary respiratory alkalosis
Alkalemia, respiratory acidosis, metabolic alkalosis, and hypoxia
Acidosis with compensatory hypoventilation
Long-term metabolic compensation for respiratory alkalosis
An 8-year-old boy is seen in the pediatrician's office for a routine health supervision visit. The mother states that he has Duchenne muscular dystrophy. On examination, he is found to have hip waddle and enlargement of both calves. He is ambulatory, but his muscle strength is diminished symmetrically. Which of the following signs is most consistent with Duchenne muscular dystrophy?
Myotonia
"Foot drop" gait
Gower sign
Positive Babinski sign
Increased deep tendon reflex
A 9-year-old boy is brought to the pediatrician's office for bed-wetting. His mother states that he has never been dry at night. Occasionally, he has problems controlling his bladder during the day. On physical examination, his blood pressure is 98/56 mm Hg. Both his weight and height are below the 5th percentile for his age. His bladder is enlarged and palpable above the symphysis pubis. Which of the following is the most likely cause of his problem?
Reflux nephropathy
Unstable bladder
Sickle cell trait
Primary polydipsia
Obstructive uropathy
A frail 6-year-old child who has cystic fibrosis is transported by ambulance to the emergency department. She has had hemoptysis for the past 4 hours, yielding approximately 10 mL of bright red blood. She has had increased cough over the past 3 days. Physical examination findings include a respiratory rate of 38 breaths/min, heart rate of 90 beats/min, oxygen saturation of 92% on room air, blood pressure of 100/70 mm Hg, and temperature of 98.6ºF (37ºC). She is awake and alert but seems breathless when she tries to speak. On auscultation, you note diffuse crackles throughout her lung fields. Of the following, the BEST next step in the management of this patient is to
Transfuse with O-negative blood
Insert an endotracheal tube and begin positive pressure ventilation
Begin therapy with ceftriaxone
Obtain blood for determination of prothrombin and partial thromboplastin time
Administer methylprednisolone
A child can walk well holding on to furniture but is slightly wobbly when walking alone. She uses a neat pincer grasp to pick up a pellet, and she can release a cube into a cup after it has been demonstrated to her. She tries to build a tower of two cubes with variable success. She is most likely at which of the following age?
4 months
1 year
6 months
2 months
9 months
A 7 year old with a 3-day history of upper respiratory tract infection is brought to accident and emergency by his mother because he suddenly went pale and sweaty and seems to be working hard to breath. The triage nurse calls you to see him urgently because his heart rate is 200 beats per minute. You take him round to the resuscitation area, give him oxygen and connect him to the cardiac monitor. The electrocardiogram (ECG) shows a narrow complex tachycardia with a rate of 180 beats per minute. He remains alert, with a respiratory rate of 40. What is the most appropriate initial diagnosis?
Atrial fibrillation
Supraventricular tachycardia (SVT)
Wolff–Parkinson–White syndrome
Ventricular fibrillation
Ventricular tachycardia
A 41-year-old woman who is 32-weeks pregnant presents to the emergency department in labor. Her pregnancy has been complicated by gestational hypertension. Her medical history is otherwise unremarkable. She does not abuse alcohol, tobacco, or illicit drugs. Despite medical interventions, her preterm labor cannot be arrested, and she delivers a 2 kg (41b, 5oz) female infant. Both she and the child do well after delivery. Which of the following is true regarding immunizations for this infant?
Immunizations should be started after she reaches 3 kg
Immunizations should be given when allergen testing confirms an immune response
Immunizations should be given according to the gestational age
Toxoid and polysaccharide vaccines should be given according to chronologic age, but live attenuated vaccines should be given according to the gestational age
Immunizations should be given according to the chronologic age

The infant in the following picture presents with hepatosplenomegaly, anemia, persistent rhinitis, and a maculopapular rash. Which of the following is the most likely diagnosis for this child?
Glycogen storage disease
Congenital syphilis
Cytomegalovirus disease
Toxoplasmosis
Congenital hypothyroidism
A 1-week-old infant presents for his first newborn evaluation. He had been discharged apparently well and thriving at 48 hours of age. He now exhibits grouped vesicles on an erythematous base that were not present at birth. Wright stain of scrapings from the floor of the vesicles reveals multinucleated giant cells and balloon cells. Of the following, the MOST likely diagnosis is
Bullous impetigo
Congenital varicella
Recessive dystrophic epidermolysis bullosa
Herpes simplex virus infection
Incontinentia pigmenti
A 6-week-old male infant, who was born at 32 weeks' gestation with a birth weight of 1500 g, has had an average weight gain of 8 g/day since birth. He takes an iron-fortified formula that is 24kcal/oz. His calorie intake is about 125kcal/day. It is noted that his stool is poorly formed and bulky. Which of the following dietary modifications will most likely result in decreased steatorrhea and improved weight gain?
Change to a lactose-free formula
Supplement with vitamins A and E
Add pancreatic enzymes to the formula
Substitute medium-chain triglycerides for long-chain triglycerides
Increase calorie intake to 175 kcal/day by increasing volume per feed
A one-and-a-half-year-old Caucasian child is referred to paediatrics for failure to thrive. On examination he is a clean, well-dressed child who is quite quiet and withdrawn. He is pale and looks thin with wasted buttocks. His examination is otherwise unremarkable. What is the most likely cause of this child’s growth failure? His growth chart shows good growth along the 50th centile until 6 months followed by weight down to the 9th, height down to 25th and head circumference now starting to falter at 1.5 years.
Constitutional delay
Coeliac disease
Normal child
Neglect
Beta thalassaemia
A previously healthy 18-month-old has been in a separate room from his family. The family notices the sudden onset of coughing, which resolves in a few minutes. Subsequently, the patient appears to be normal except for increased amounts of drooling and refusal to take foods orally. Which of the following is the most likely explanation for this toddler’s condition?
Foreign body in the esophagus
Epiglottitis
Severe gastroesophageal reflux
Foreign body in the airway
Croup
A 15-year-old boy presents with melena and anemia. Endoscopy demonstrates a nodular gastritis of the antrum and an ulcer. Biopsies of the antrum demonstrate spiralshaped organisms consistent with Helicobacter pylori. You prescribe amoxicillin, clarithromycin, and lansoprazole for 2 weeks. At a follow-up visit, the family asks whether the treatment has been successful in eradicating the organism. Of the following, the PREFERRED noninvasive test to evaluate whether the pathogen has been eradicated is
Fecal Campylobacter-like organisms (CLO) test
Fecal H pylori antigen
Serum H pylori urease concentrations
Salivary H pylori antibody concentrations
Serum H pylori immunoglobulin G serology
A child presents for her 2-week evaluation after being delivered by a midwife at home. The parents are concerned that they have never seen her turn her head, which makes it difficult for her to feed at the breast. They also note that her back does not appear normal. On physical examination, her hairline appears low posteriorly. You confirm that she does not turn her head, and when placed prone, does not turn her head to the side. Her right scapula appears to be higher than the left, and you note that the spine does not appear to be perfectly straight, suggesting congenital scoliosis. You obtain an anteroposterior radiograph of the cervical spine, which shows multilevel segmentation anomalies (Item Q165A) in the mid to lower cervical spine. Of the following, the condition that is MOST consistent with these findings is
Noonan syndrome
Turner syndrome
Sandifer syndrome
Cleidocranial dysostosis
Klippel-Feil syndrome
A 21-year-old woman presents to the emergency room in active labor. She has had no prenatal care, but her last menstrual period was approximately 9 months prior. Her membranes are artificially ruptured, yielding no amniotic fluid. She delivers an 1800-g (4-lb) term infant who develops significant respiratory distress immediately at birth. The first chest radiograph on this infant demonstrates hypoplastic lungs. After this infant is stabilized, which of the following is the most appropriate next step for this infant?
Liver and spleen scan
Renal ultrasound
Upper GI
MRI of the brain
Cardiac catheterization

You are seeing a 4-year-old girl with the physical examination finding shown below. She has no significant past history. The most appropriate management is which of the following?
Surgical consultation for correction
Topical estrogen cream daily for a week
Referral to social services for possible sexual abuse
Karyotypestudies
Topical steroid cream for a week
A 28-year-old Caucasian female comes to the office due to fever for the past 3 days. She also complains of pain and swelling in her right breast for the past 4 days. She exclusively breastfeeds her 3-month-old baby. On examination, she is febrile. Her right breast is engorged, red and tender, without any area of fluctuation. She wants to know if she can continue to breastfeed. Which of the following is a contraindication to breastfeeding?
Acquired immune deficiency syndrome
Hemolytic disease of the newborn
Mastitis
Maternal rubella infection
Breast milk jaundice
A mother brings her infant into the clinic for a routine visit. Examination reveals nothing abnormal. Developmental assessment shows that the infant sits well unsupported, enjoys looking around, babbles, and has a raking grasp. What is the most likely age of this infant?
4 months
6 months
8 months
10 months
12 months
A 15-year-old Caucasian male is brought to the office by his mother for the evaluation of a six-month history of unstable gait and speech difficulty which are getting worse over time. His past medical history is insignificant. He is not taking any medications, and denies smoking or alcohol consumption. His blood pressure is 120/70 mmHg and pulse is 80/min. Musculoskeletal examination showed scoliosis and feet deformity with 'hammer toes.' The neurologic examination showed dysarthria, dysmetria, nystagmus, and absence of deep plantar reflexes on lower extremities. What is the most common cause of death in this patient population?
Renal failure
Diabetes-related complications
Cardiomyopathy
Septic shock
Malignancy
A 15-year-old girl is admitted to the hospital with a 6-kg weight loss, bloody diarrhea, and fever that have occurred intermittently over the previous 6 months. She reports cramping abdominal pain with bowel movements. She also reports secondary amenorrhea during this time. Stool cultures in her physician’s office have shown only normal intestinal flora. A urine pregnancy test was negative, while an erythrocyte sedimentation rate (ESR) was elevated. Her examination is significant for the lack of oral mucosal ulcerations and a normal perianal examination. Anti-Saccharomyces cerevisiae antibodies (ASCA) are negative, while anti-neutrophil cytoplasm antibodies (pANCA) are positive. You confirm your presumptive diagnosis with a rectal biopsy. In counseling her about her disease, which of the following statements would be true?
The most serious complication of her disease is toxic megacolon
Intestinal strictures are common
Inheritance is autosomal dominant
The intestinal involvement is separated by areas of normal bowel
Her risk of colon cancer is minimally elevated over the general population
The father of three children in your practice recently was diagnosed with Crohn disease. His wife does not have Crohn disease. He asks you if his children, ages 10, 12, and 16 years, are at increased risk for developing the same illness. Of the following, you are MOST likely to advise the father that
Crohn disease in childhood usually presents in children younger than age 5 years
Smoking is associated with an increased risk of developing Crohn disease
Although his children are at increased risk of developing Crohn disease, their risk of developing ulcerative colitis is decreased
Most patients who have Crohn disease can be diagnosed by genetic testing
Each of his children has at least a 20% chance of developing Crohn disease during his or her lifetime
In examining a 4-year-old girl who is new to your practice, you discover that she has rudimentary thumbs and is well below the 5th percentile for both weight and height. You also observe irregular hyperpigmentation on the trunk and anogenital areas. Of the following, the MOST likely hematologic disorder associated with these findings is
Diamond-Blackfan anemia
Fanconi anemia
Bloom syndrome
Acute lymphoblastic leukemia
Thrombocytopenia and absent radii (TAR) syndrome
A 4-year-old girl is brought to the office due to easy bruising and a rash for the past 3 days. She had an upper respiratory infection approximately two weeks ago. She has never had palpable bruises, hemarthroses, or deep muscle bleeding in the past. She has 2 older brothers, neither of which has had bleeding symptoms before. Her family history is negative for any bleeding disorders. Her vital signs are normal. Physical examination reveals a diffuse petechial rash on her neck, trunk, extremities and groin. There is no hepatosplenomegaly. Nonpalpable ecchymoses of varying ages are present on the shins and arms. The laboratory findings are as follows: Hemoglobin 12 .8 g/dl, Hematocrit 38.5%, WBC 6,000/mm3, Platelets 5,000/mm3, PT 12.0 sec, PTT 30 sec. Peripheral smear shows normal morphology of the red and white blood cell lines. The platelets are reduced in number, and majority of them are increased in size. What is the most likely diagnosis?
Hemolytic uremic syndrome
Immune thrombocytopenic purpura
Von Willebrand's disease
Thrombotic thrombocytopenic purpura
Hemophilia
A 6-year-old girl presents to accident and emergency with a fever. She has no history of cough, cold, vomiting, diarrhoea, rash, headache or joint pain. On examination, she is tachycardic at 150 bpm and there are two petechial spots on her right ankle. Her capillary refill time is 4 seconds and she has cold feet. All her other observations are normal. What is the most appropriate course of action?
IV fluid bolus and IV ceftriaxone
Discharge home and advise to return if the rash spreads
Admit to the ward for observation
IV ceftriaxone
Inform the consultant about child protection concerns
A 16-year-old girl presents to your office with a recent diagnosis of peptic ulcer. The gastroenterologist has prescribed sucralfate. Of the following, the condition that is a relative contraindication to sucralfate treatment is
Congenital heart disease
Steroid-dependent asthma
Congenital hepatic fibrosis
Diabetes mellitus
End-stage renal disease
A young black male with sickle cell trait is preparing for his travel to West Africa from North America. While obtaining his visa, he is advised by the health inspector to obtain some immunizations, although his chances of getting a certain tropical disorder are low. What disease has the sickle cell trait been shown to convey protection against?
Tuberculosis
Lymphoma
Malaria
Histoplasmosis
Leprosy
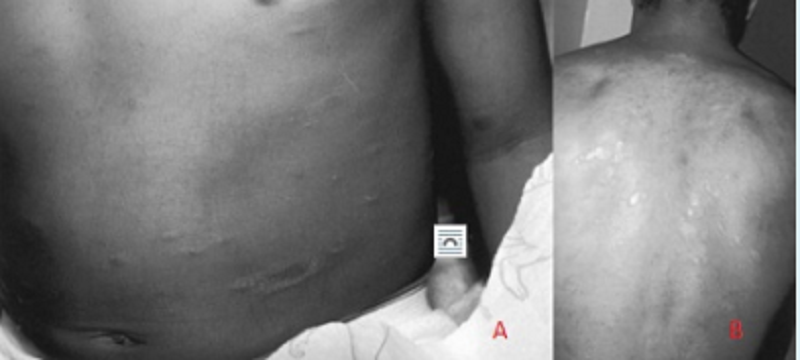
The adolescent shown presents with a 14-day history of multiple oval lesions over her back. The rash began with a single lesion over the lower abdomen (Image A); the other lesions developed over the next days (image B). These lesions are slightly pruritic. Which of the following is the most likely diagnosis?
Seborrheic dermatitis
Lichen planus
Psoriasis
Contact dermatitis
Pityriasis rosea
An 8-year-old boy presents to your office for a second opinion. He has a 2-year history of intermittent vomiting, dysphagia, and epigastric pain. His father reports he occasionally gets food “stuck” in his throat. He has been on a proton pump inhibitor for 18 months without symptom relief. His past history is significant only for eczema and a peanut allergy. Endoscopy was performed 6 months ago; no erosive lesions were noted and a biopsy was not performed. You arrange for a repeat endoscopy with biopsy. Microscopy on the biopsy sample reveals many eosinophils. Treatment of this condition should include which of the following?
Prolonged acid blockade
Corticosteroids
Treatmentfor Aspergillus sp
Observation
Treatment for Candida sp
You see a boy in outpatients whose parents are concerned he is not talking yet. You do a developmental assessment and find he is walking well and able to build a tower of three blocks. He will scribble but does not copy your circle. He is able to identify his nose, mouth, eyes and ears as well as point to mummy and daddy. You do not hear him say anything but his parents say he will say a few single words at home such as mummy, daddy, cup and cat. He is a happy, alert child. Parents report him to be starting to feed himself with a spoon and they have just started potty training but he is still in nappies. What is the child’s most likely age?
2 years
15 months
2.5 years
18 months
12 months
A 12-year-old male is brought to your office by his mother because of a several month history of back pain. He also experienced bed wetting recently. His past medical history is insignificant. He tried acetaminophen for pain relief. He does not smoke or consume alcohol. His temperature is 36.7 C (98 F), blood pressure is 110/65 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals a palpable "step off" at the lumbosacral area. Straight-leg raising test is negative on both sides. Perianal sensation tested by pinprick test is decreased, but anal reflex is normal. What is the most probable diagnosis in this patient?
Lumbosacral strain
Spondylolisthesis
Multiple myeloma
Compression fracture of the vertebrae
Ankylosing spondylitis
A 7-year-old boy is brought to the physician because of a persistent mucopurulent nasal discharge for 2 weeks following a common cold. The mother also reports that the child has had frequent cough during the day and occasional temperatures up to 38.0 C (100.5 F). The child does not appear critically ill, but he complains of mild pain in the maxillary region and nasal obstruction. Rhinoscopic examination reveals a rivulet of purulent fluid coming from the inferior meatus. The rest of the physical examination is normal. Which of the following is the most likely diagnosis?
Acute otitis media
Acute bacterial sinusitis
Allergic rhinosinusitis
Asthma
Acute viral rhinitis
An obese Caucasian father brings his 1 0-year-old obese son to your office. The father states that he was recently diagnosed with high cholesterol levels and coronary artery disease. Even though his son is asymptomatic, he is worried about the obesity. Which of the following best explains the next best step in management?
Get a screening test for total cholesterol level
Advise parents to start him on a regular physical exercise schedule
Advise parents to start him on a low cholesterol diet
Evaluate him for coronary artery disease
Get a fasting lipid profile
A young mother claims that her 4-week-old child sleeps best on his stomach. You tell her that the safest sleep position for infants is which of the following?
On the back
In the parents’ bed
On the side
On the stomach
On the back with the head elevated by a pillow
A 16-year-old boy presents with a very swollen, painful right knee. He is a soccer player, but there is no history of recent injury. During the interview, you notice the boy has injected conjunctivae. Of the following, further evaluation MOST likely will reveal
Gottron papules
Malar rash
Urethritis
Alopecia areata
Kayser-Fleischer rings
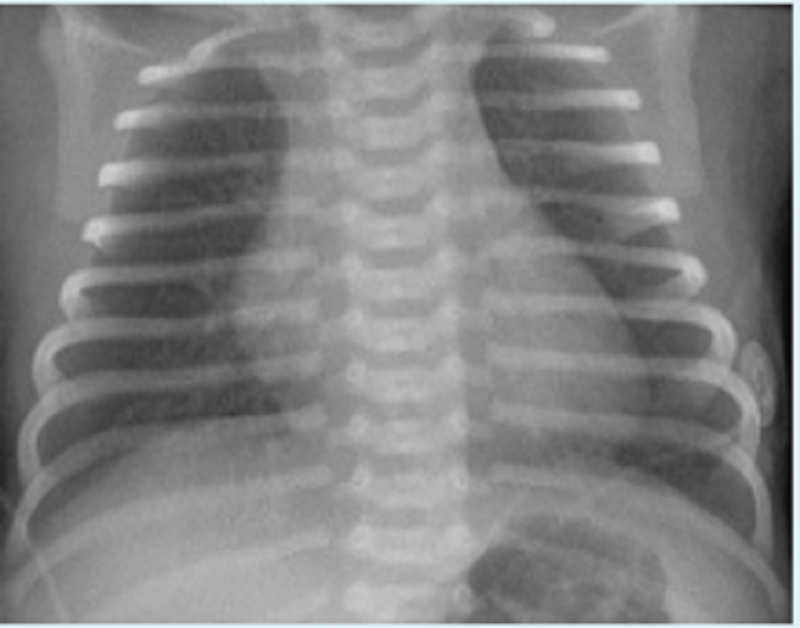
An infant weighing 1400 g (3 lb) is born at 32 weeks’ gestation. Initial evaluation was benign, and the infant was transferred to the level 2 nursery for prematurity. The nurse there calls at 1 hour of life and reports the infant is tachypneic. Vital signs include a heart rate of 140 beats per minute, a respiratory rate of 80 breaths per minute, a temperature of 35°C (95°F), and a peripheral oxygen saturation of 98%. The lungs are clear with bilateral breath sounds and there is no murmur; the infant is in no dis- tress. The child’s chest radiograph is shown. Which of the following is the most appropriate next step in evaluating the infant?
Obtain a complete blood count and differential
Administer supplemental oxygen
Place the infant under a warmer
Administer intravenously 5cc of D50W
Perform a lumbar puncture
A 9-month-old infant is brought to the emergency department with lethargy and tachypnea. He was healthy before developing fever and diarrhea four days ago. He has been taking some formula, but has had two to three episodes of diarrhea with each bottle. He has lost three pounds (1 .4 kg) since his routine check-up two weeks ago. He has had one wet diaper in the past twenty four hours. On examination, his temperature is 102.5F (39.1c), pulse is 200/min, respiratory rate is 42/min, and blood pressure is 70/45 mm Hg. He is lethargic with decreased tone and decreased deep tendon reflexes. His mucous membranes are dry. Cardiopulmonary exam reveals tachycardia and tachypnea. His abdominal exam is unremarkable. Capillary refill is four seconds. Laboratory results are shown below. Chemistry panel: Serum sodium 165 mEq/L, Serum potassium 4.5 mEq/L, Chloride 108 mEq/L, Bicarbonate 14 mEq/L, Blood urea nitrogen (BUN) 20 mg/dl, Serum creatinine 0.8 mg/dl, Calcium 10.0 mg/dl, Blood glucose 98 mg/dl. Which of the following fluids should be used as a bolus in the resuscitation of this infant?
0.45% saline
0.9% saline
5% dextrose
Packed red blood cells
5% albumin
A primiparous woman whose blood type is O positive gives birth at term to an infant who has A-positive blood and a hematocrit of 55%. A total serum bilirubin level obtained at 36 hours of age is 12 mg/dL. Which of the following additional laboratory findings would be characteristic of ABO hemolytic disease in this infant?
Crescent-shaped red blood cells in the blood smear
A normal reticulocyte count
A positive direct Coombs test
Elevated hemoglobin
Petechiae
A 4-year-old previously well African American boy is brought to the office by his aunt. She reports that he developed pallor, dark urine, and jaundice over the past few days. He stays with her, has not traveled, and has not been exposed to a jaundiced person, but he is taking trimethoprim sulfamethoxazole for otitis media. The CBC in the office shows a low hemoglobin and hematocrit, while his “stat” serum electrolytes, blood urea nitrogen (BUN), and chemistries are remarkable only for an elevation of his bilirubin levels. His aunt seems to recall his 8-year-old brother having had an “allergic reaction” to aspirin, which also caused a short-lived period of anemia and jaundice. Which of the following is the most likely cause of this patient’s symptoms?
Hepatitis B
Gilbert syndrome
Glucose-6-phosphate dehydrogenase deficiency
Hepatitis A
Hemolytic-uremic syndrome
A 7 -day-old male infant is brought by his mother complaining of decreased movements of his right arm. She denies any trauma or fall. Pregnancy was uneventful, but delivery was complicated with shoulder dystocia. Examination reveals the presence of crepitus and bony irregularity over the clavicular area and Mora reflex is absent on the right. Which of the following is the most appropriate management?
Casting of the right arm and shoulder
Reassurance
Nerve grafting
Figure-of-eight clavicle strap
Passive and active motion exercises
An 11-month-old girl is brought by her mother to the office due to fever, fussiness, and irritability. The girl has a tendency to hold and pull on her left ear. For the past few days, she has had rhinorrhea and nasal congestion. Her medical history reveals nothing particular. Her temperature is 38.9C (102F). Otoscopic examination reveals a bulging, erythematous tympanic membrane with decreased mobility on air compression. What is the most likely organism responsible for the patient's condition?
Group A Streptococcus
Pseudomonas aeruginosa
Haemophilus influenzae
Streptococcus pneumoniae
Moraxella catarrhalis
A 12-year-old African American male with known sickle cell disease presents with a 2 hours history of right-sided arm weakness ans slurred speech. He has been hospitalized before for pain crises and pneumonia. He takes hydroxyurea, oxycodones as needed, and folic acid. His temperature is 36.6 C, BP is 153/83 mmHg and HR is 112/min with regular rhythm. On physical examination, he has right arm weakness and mild dysarthria. His laboratory values are the following: Hemoglobin 8.2 mg/dL, WBC count 14, 000.mm3, Platelet count 210, 000/mm3, Creatinine 0.9 mg/dL. CT of the head shows no evidence of intracranial bleeding. Which of the following is the best initial management for this patient?
Exchange transfusion
Plasmapheresis
Beta blockers and aspirin
Fibrinolytic therapy
Heparin and warfarin
A 10-year-old male fell while riding his scooter down a steep hill. In the Emergency Department, his injuries included a fractured wrist and a lacerated spleen, which required surgical removal. Two years later he is diagnosed with bacterial pneumonia. Which of the following bacterial agents is the most likely pathogen for this patient's pneumonia?
Neisseria meningitidis
Streptococcus pneumoniae
Klebsiella pneumoniae
Escherichia coli
Staphylococcus aureus
A mentally retarded 14-year-old boy has a long face, large ears, micropenis, and large testes. Chromosome analysis is likely to demonstrate which of the following?
Trisomy 21
Trisomy 13
Fragile X syndrome
Trisomy 18
Williams syndrome
You are evaluating a newborn boy who has lax abdominal musculature and bilateral undescended testes. Other findings on physical examination are normal. Of the following, the MOST likely urologic abnormality in this boy is
Ureterocele
Vesicoureteral reflux
Renal cysts
Hydronephrosis
Ureteropelvic junction obstruction
An 18-month-old boy is brought to the clinic for a checkup. As part of his routine care, a serum lead level is obtained. It is 25 g/mL. Which of the following is the most appropriate next step in his management?
Chelation with succimer
Investigation of his home for lead hazards
Reassurance that this level is not a problem
Chelation with CaEDTA
Repeating the level in 6 months
A 15-year-old is participating in high school football practice in August in Texas. He had complained of headache and nausea earlier in practice, but kept playing after a cup of water. He is now confused and combative. He is dizzy and sweating profusely. His temperature is 41°C (105.8°F). Therapy should consist of which of the following?
Initiate whole body cold water immersion
Tell him to go take a shower and rest until the next day’s practice
Administer acetaminophen rectally
Order to rest on the bench until symptoms resolve
Provide oral rehydration solutions
An 8-year-old immigrant from rural Central America presents with complaints of weakness, facial swelling, muscle pain, and fever. A CBC reveals marked eosinophilia. Which of the following parasites is most likely to be responsible?
Enterobius vermicularis
Giardia lambila
Trichinella spiralis
Cryptosporidium parvum
Sporothrix schenckii
An 8-year-old girl presents with well-controlled, moderately persistent asthma. Her therapies consist of occasional use of short-acting β-agonists, daily inhaled steroids, and a leukotriene inhibitor. She presents with white patches on her buccal mucosa. You recommend which of the following?
Discontinuation of all her asthma medications
HIV testing
Tuberculosis skin testing
Measurement of serum immunoglobulins
Rinse her mouth after use of her inhaled medications
A preterm baby is born at 25 + 6 weeks gestation. He is delivered by caesarean section due to maternal pre-eclampsia. He is intubated at birth and given surfactant via the endotracheal tube. He is ventilated and commenced on IV dextrose. After 4 hours of age he has increased work of breathing, with intercostal and subcostal recession and a respiratory rate of 60/min. A chest x-ray shows a ground glass pattern in both lung fields. He has no audible murmur. He is afebrile. You diagnose respiratory distress syndrome. What is the aetiological factor responsible for respiratory distress syndrome?
Lung hypoplasia
Infection with group B Streptococcus
Pneumonitis
Immature lung parenchyma
Surfactant deficiency
A 1-year-old presents for a well-child checkup, but the parents are concerned about giving the child his immunizations. Which of the following is a true contraindication to the administration of the fourth DTaP (diphtheria and tetanus toxoid and acellular pertussis) vaccine?
A past history of infantile spasms
Prolonged seizures 6 days after the last DTaP vaccine
Child is currently febrile to 39 C (102.2 F)
Positive family history of adverse reactions to DTaP vaccine
Child is currently on amoxicillin for an otitis media
A 3-year-old boy is brought to the emergency department because of a worsening cough over the past week. His temperature is 38.9 C (102 F), and inspiratory stridor is noted. A plain film of the neck reveals subglottic swelling. He is noted to have copious thick secretions and a barking cough. He has not had such events previously, and his parents deny recent contact with sick children. The patient is in respiratory distress and is noted to be retracting his subcostal muscles to breathe. Which of the following is the next most appropriate step in management?
Administer albuterol
Administer IV penicillin
Endotracheal intubation
Administer corticosteroids
Administer racemic epinephrine
A 2-month-old girl presents to her pediatrician's office for well-child care. Her mother complains of excessive tearing of the baby's left eye for the past 4 weeks. Each morning, a yellow crusty discharge is noted along the lashes of the left eye. The conjunctiva appears uninflamed. The right eye is not affected. On physical examination, the infant is otherwise well and achieving adequate weight gain on an exclusive breast milk diet. She is developmentally appropriate, including visually tracking 180 degrees. Which of the following is the most likely diagnosis?
Vitamin A deficiency
Viral conjunctivitis
Dacryostenosis
Normal infant eye
Gonococcal conjunctivitis
A 3-week-old baby is brought to the ‘prolonged jaundice clinic’. His mother reports he has poor feeding, is not gaining weight appropriately and is more sleepy compared to her previous child. He opens his bowel once a day and is being mix breast and bottle fed. He is floppy, jaundiced, has a large, protruding tongue and a hoarse cry. He had a newborn blood spot screening test done at birth which was normal and he has no dysmorphic features. What is the most likely diagnosis of this child?
Beckwith–Wiedemann syndrome
Normal baby
Down’s syndrome
Congenital hypothyroidism
Prader–Willi syndrome
A 14-year-old girl is brought to the physician’s office because of irregular menstrual periods. She had her menarche at age 13, and since then her periods have been irregular with the cycles varying from 3 to 6 weeks. She has no other symptoms. Physical examination is unremarkable. She has age appropriate secondary sexual characteristics. A urine pregnancy test is negative. Serum prolactin and thyroid stimulating hormone levels are normal. Administration of micronized oral progesterone results in withdrawal bleeding in 3 days. Which of the following most likely explains her irregular periods?
Uterine adhesions
Marked estrogen deficiency
Marked androgen excess
Excess LH secretion
Insufficient gonadotropin secretion
A 4-week-old infant presents with tachycardia, tachypnea, and poor weight gain. His arterial blood gas shows a pH of 7.34, a PaCO2 of 41 mm Hg, and a PaO2 of 74 mm Hg. A chest radiograph shows cardiomegaly. Echocardiography reveals a structurally normal heart, left ventricular dilatation, a left ventricular ejection fraction of 20%, and mild mitral and tricuspid regurgitation. IV administration of which of the following medications is the best initial step in management of this patient?
Furosemide
Corticosteroid
Angiotensin-converting enzyme inhibitor
Epinephrine
Digoxin
A 12-year-old boy comes to the emergency department at midnight with a complaint of severe scrotal pain since 7 PM. There is no history of trauma. Which of the following is the most appropriate first step in management?
Order a surgical consult immediately
Order a radioisotope scan as an emergency
Arrange for an ultrasound examination
Order a Doppler examination
Order a urinalysis and Gram stain for bacteria
A 3-year-old girl presents to the pediatrician's office. The mother states that the girl has been having big, bulky stools that float in the toilet. She also has intermittent diarrhea. On examination, her height is 88 cm (34.6 in, <5th percentile) and weight is 15.8 kg (34.8 lb, <5th percentile). In addition, she has an uncle who died of recurrent lower respiratory infections. Which of the following would be most effective for alleviating the gastrointestinal symptoms of this patient?
Oral metronidazole
Avoidance of dairy products
Ketogenic diet
Elimination of dietary fat
Pancreatic enzyme replacement
Examination of the cerebrospinal fluid (CSF) of an 8-year-old, mildly febrile child with nuchal rigidity and intermittent stupor shows the following: WBCs 85/µL (all lymphocytes), negative Gram stain, protein 150 mg/dL, and glucose 15 mg/dL. A computed tomographic (CT) scan with contrast shows enhancement of the basal cisterns by the contrast material. Which of the following is the most likely diagnosis?
Tuberous sclerosis
Stroke
Acute bacterial meningitis
Tuberculous meningitis
Pseudotumor cerebri
A 3-year-old boy is brought to the physician for help with toilet training. He recently started day care and screams "no" when teachers try to place him on the toilet. He has bowel movements every other day and strains when he passes hard, pellet-like stools. The boy is a picky eater but loves milk and drinks up to 30 oz of chocolate milk daily. He has no medical problems and takes no medications. His weight and height have been tracking along the 75th percentile. Examination shows a cooperative, well-nourished boy. He runs well and can climb onto the examination table independently. He speaks in short sentences that are mostly understandable. The boy's abdomen is soft, nontender, and nondistended. He has normal Tanner I male genitalia. A small fissure is noted on the anal verge. Which of the following is the best next step in management of this patient?
Anorectal manometry
Increase juice intake
Disimpaction with rectal enema
Oral laxative therapy
Abdominal x-ray
An 18-month-old boy has received 5 days of amoxicillin for otitis media. He continues to have fever, and on physical examination, the right tympanic membrane is bulging with purulent fluid behind it. Which of the following is the best antibiotic to use?
Cephalexin
Penicillin
Amoxicillin-clavulanic acid
Erythromycin
Dicloxacillin
A 12-year-old boy presents with an intensely pruritic rash for 3 days. He just went on a camping trip, during which he wore only shortsleeve shirts and short pants. His temperature is 37.6 C (99.7 F), blood pressure is 96/62 mm Hg, pulse is 65/min, and respirations are 12/min. There are numerous erythematous papules and vesicles on both arms and legs. Most of them are in a linear array. Which of the following is the most appropriate pharmacotherapy?
Topical diphenhydramine
Topical 1% hydrocortisone
Oral cephalexin
Oral prednisone
Topical mupirocin
A 3-year-old girl is brought to the pediatrician with complaints of abdominal pain and fever. Her mother states that the fever started 2 days ago, with the highest temperature being 39.0 C (102.2 F). She has had no vomiting or diarrhea. The mother states that her daughter has been complaining of pain on urination. On examination, she is tender in her lower abdomen, and there is some right-sided costovertebral angle tenderness. A urinalysis confirms the suspicion of a urinary tract infection. Which of the following would be the most appropriate diagnostic procedure?
Voiding cystourethrogram (VCUG) now
Cystoscopy
Intravenous pyelogram
Dimercaptosuccinic acid (DMSA) scan in 1-2 months
VCUG in 1-2 months
The mother of a 2-year-old boy comes to the physician because her child awakens at night, with a blank gaze, screaming in bed without recognizing his parents. These episodes have occurred three times in the past 2 weeks, always in the first few hours of the night. The child goes back to sleep and seems to retain no memory of the episode the next morning. Which of the following is the most appropriate next step in management?
Behavioral therapy
Therapy with chloral hydrate
Avoidance of TV before going to bed
Therapy with a tricyclic antidepressant
Reassurance of parents about the nature of these manifestations
A nurse asks you to examine a 26-hour-old infant who recently developed a rash. On physical examination, you note erythematous macules over the trunk, face, and proximal extremities. Most of the macules have tiny central pustules. The infant is breastfeeding well, and the remainder of the physical examination findings are normal. No lesions were present at birth. Of the following, analysis of the pustular contents is MOST likely to reveal
Pseudohyphae and budding yeast
Multinucleated giant cells
Eosinophils
Polymorphonuclear leukocytes
Gram-positive cocci
A previously healthy 4-year-old child is brought to the physician for a school physical for kindergarten. His mother has brought in his immunization record and reports that received all his immunizations prior to age 2. He has received only a yearly influenza vaccine since age 2. His physical examination is unremarkable. Which of the following immunizations should he be given during this visit?
Pneumococcal #3
Hepatitis B #3
Measles-mumps-rubella #1
Haemophilus influenza type B #4
Inactivated polio #4
A mother brings her 3-year-old son to the pediatrician because he has had 7 days of fever and a painful swollen lymph node in his right groin. This is the boy's sixth episode of lymph node swelling; previous episodes resolved after drainage and prolonged antibiotic therapy. The child also has a past medical history significant for pneumonia at 12 months of age that required chest tube placement for drainage. His maternal uncle died in childhood from recurrent infections. On examination, the boy is at the 5th percentile for both height and weight His temperature is 38.5 c (101.3 F). There is an enlarged, tender lymph node in the right inguinal area with erythema and warmth of the overlying skin. There are several healed incisions in the inguinal regions bilaterally, as well as around the neck from old drainage sites. Laboratory analyses reveal the following: Hematocrit 35%, Platelet count 350,000/mm3, Leukocyte count 17000/mm3, Segmented neutrophils 65%, Bands 10%, Lymphocytes 25%. Gram stain of fluid aspirated from the affected lymph node reveals numerous bacteriafilled segmented neutrophils. Cultures grow S. aureus. What is the most likely mechanism underlying these findings?
Defective opsonization
Destruction of CD4+ lymphocytes
Impaired oxidative metabolism within phagocytes
Adenosine deaminase deficiency
Complement consumption
A woman gives birth to twins at 38 weeks’ gestation. The first twin weighs 2800 g (6 lb, 3 oz) and has a hematocrit of 70%; the second twin weighs 2100 g (4 lb, 10 oz) and has a hematocrit of 40%. Which of the following statements is correct?
The second twin is at risk for developing respiratory distress, cyanosis, and congestive heart failure
The second twin is at risk for renal vein thrombosis
The second twin is likely to be pale, tachycardic, and hypotensive
The first twin is more likely to have hyperbilirubinemia and convulsions
The second twin probably has hydramnios of the amniotic sac
A term newborn is delivered by emergent cesarean section because of intrauterine growth restriction, oligohydramnios, and nonreassuring fetal heart rate monitoring in labor. Delivery room resuscitation includes endotracheal intubation and assisted ventilation with 100% oxygen, chest compressions, intravenous epinephrine, and volume expansion. Apgar scores are 1, 2, and 3 at 1, 5, and 10 minutes, respectively. An umbilical cord arterial blood gas measurement documents a pH of 6.9 and a base deficit of 20 mmol/L. At 12 hours of age, the infant demonstrates tonic-clonic convulsive activity of the arms and legs with a concomitant decrease in heart rate and bedside pulse oximetry saturation. Of the following, the MOST likely cause for this infant's seizure is:
Hypercarbia
Hyperglycemia
Hypercalcemia
Hypomagnesemia
Hypoxia
A 4-month-old is brought to clinic by his parents for evaluation of bilateral droopy eyes. His mother believes this has developed just over the last week. The child recently started taking cereal in addition to breastfeeding and has been constipated. Physical examination reveals droopy eyelids and 1+ deep tendon reflexes diffusely. Of the following, the MOST likely diagnosis is
Muscular dystrophy
Botulism
Myasthenia gravis
Blepharophimosis syndrome
Congenital ptosis
A blood type B infant born to a blood type O mother has clinically significant fetal-maternal blood group incompatibility with mild anemia and a weakly positive Coombs test. The infant develops jaundice a few hours after birth, with a bilirubin (measured at 12 hours after birth) of 12 mg/dL (predominately unconjugated) compared with 3.5 mg/dL in cord blood. The physician is concerned that the rising bilirubin levels will damage the infant's nervous system. Which of the following sites is most vulnerable to this injury?
Peripheral nerve
Spinal cord
Cerebellum
Cerebral cortex
Basal ganglia
You are evaluating a 2-year-old boy in your office for recurrent cellulitis of his right thigh. The patient has had three episodes in the last 4 months. According to his mother, all the episodes start with a "red bump" that progressively enlarges and, in most cases, drains spontaneously. He has received two courses of cephalexin in the past, but there was no clinical improvement until the abscess spontaneously drained. On one occasion, an incision and drainage procedure had to be performed. Except for pain with walking, the patient has been afebrile and experienced no other systemic symptoms. On physical examination, you note a 6x6 cm area of induration and erythema on the lateral right thigh that is warm, firm, and tender to palpation. There is no active drainage from the site. Of the following, the MOST appropriate antibiotic for treatment of this patient is
Amoxicillin/clavulanic acid
Amoxicillin
Cefdinir
Cephalexin
Clindamycin

A 2-day-old boy in the newborn nursery was born at 39 weeks gestation to a 38-year-old woman by vaginal delivery. The mother received epidural fentanyl for severe painful contractions during labor, but the delivery was uncomplicated. Since birth, the boy has shown little interest in breast or bottle feeding. He spit up the last feed but has not vomited. He has not yet passed meconium. Physical examination shows a newborn with generalized hypotonia, a flat facial profile, low-set folded earlobes, and a single transverse crease on each palm. His abdomen is firm and distended. Digital rectal examination is notable for a tight anal canal and relieves an expulsion of gas and stool. Abdominal x-ray shows markedly distended loops of bowel with no gas in the rectum. What is the mostly likely mechanism for his findings?
Intestinal obstruction from inspissated meconium
Failure of neural crest cell migration during fetal intestinal development
Invagination of a part of the intestine into itself
Intestinal ileus from exposure to maternal epidural analgesia
Constipation from decreased levels of thyroxine
A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has difficulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds. Which of the following is the most likely age of this child?
5 years
3 years
1 year
2 years
4 years
A one-year-old girl is brought to the office for the evaluation of sickle cell anemia. Both her parents have sickle cell trait, and her elder sister has sickle cell anemia. Her vital signs are stable. Her height and weight are appropriate for age. On examination, she appears healthy and normal. Her birth and past medical histories are insignificant. Hemoglobin electrophoresis reveals 40% hemoglobin S. What is the most common presentation of this condition?
Painless hematuria
Splenic infarction
Acute painful episodes
Frequent UTI
Dactylitis
A 10-year-old boy presents to the emergency room with chief complaints of fever and increasing fatigue. He was well until 2 weeks ago when he had an upper respiratory illness (URI). He has a decreased appetite and has lost 2 lbs over the last 2 weeks. He has some shortness of breath when he climbs the stairs. His past medical history is unremarkable. On examination his vital signs are normal, and his height and weight are at the 80th percentile. His conjunctiva are pale, and he has bilateral, mobile (about 1-2cm) and non-tender nodes in the cervical, axillary, and inguinal regions. Hepatosplenomegaly is present, and skin shows no lesions. Labs are Hemoglobin 7.3g/dl, platelet count 20,000/mm3, WBC count 42,100/mm3, with 24% lymphoblasts, 70% lymphocytes, and 6% atypical lymphocytes. Chest X-rays show clear lung fields but a wide mediastinum. Which of the following is the most likely diagnosis in this patient?
Acute myeloid leukemia
Immune thrombocytopenic purpura
Hodgkin's disease
Acute lymphoblastic leukemia
Aplastic anemia
A 5-year-old boy suffers from a condition characterized by recurrent fungal and viral infections, thymic hypoplasia, tetany, and abnormal facies. Serum levels of immunoglobulins are mildly depressed, and lymph node biopsy shows lymphocyte depletion of T-dependent areas. Which of the following is the underlying pathogenetic mechanism?
In utero infection by human immunodeficiency virus (HIV)
Developmental defect of the third/fourth pharyngeal pouches
Mutations of an autosomal gene encoding adenosine deaminase
Mutations of an X-linked gene coding for a cytokine receptor subunit
Mutations of an X-linked gene coding for a tyrosine kinase
A 16-year-old African American male with sickle cell anemia presents complaining of a 1-week history of exertional dyspnea, fatigue, and generalized weakness. He denies fevers, chills, night sweats, or cough. His only medication is oxycodone for chronic pain. On physical examination, he weighs 68 kg (150 lbs) and is 168cm (66 in) tall His temperature is 36.7C (98F), blood pressure is 120/70 mm Hg, pulse is 76/min, and respirations are 18/min. All organ systems appear normal Laboratory studies show: Hematocrit 20%, Mean corpuscular volume 110 fl, Reticulocyte count 1.0%. Which of the following is the most likely mechanism underlying these findings?
Increased demand for folic acid
Adverse drug reaction
Increased demand for vitamin B 12
Gastric mucosal atrophy
Bacterial overgrowth in the small intestine
An 11-year-old highly competitive gymnast presents to your office with complaints of increasing right wrist pain over the past 2 to 3 months. She recalls no specific trauma to the wrist or arm. On physical examination, you note no swelling of the distal forearm or wrist. She has normal range of motion at the wrist. There is moderate-to-marked tenderness of the distal radius, but no tenderness more distally over the wrist joint. A radiograph of the forearm shows slight widening of the distal radial physis. Of the following, you are MOST likely to explain to the child and family that
There is no evidence for trauma to her bones
This most likely represents a wrist sprain
She must stop her training immediately
Minor pains such as this are common in athletes and should not cause alarm
This is a common injury in young gymnasts that can be overcome with an altered training regimen
A 3-year-old boy is brought to the office by his parents for the evaluation of dry eyes and photophobia. He has some difficulty in adapting to darkness. He is a very poor eater, and his diet consists mainly of canned foods, and very rarely, fresh vegetables or milk. Examination reveals dry, scaly skin, follicular hyperkeratosis in the extensor surfaces of the extremities, and dry, silver-gray plaques on the bulbar conjunctiva. What is the most likely diagnosis of this patient?
Hypervitaminosis A
Vitamin A deficiency
Scurvy
Thiamine deficiency
Ariboflavinosis

A 4-year-old boy presents to the physician with fever and a sore throat. His illness began with rhinorrhea, cough, and congestion one week ago, but in the last 24 hours he has developed fever, a sore throat, and neck pain. His mother also reports that he sounds hoarse. His appetite is decreased and he complains of dysphagia. His temperature is 39.7 C (103.5F), pulse is 100/min, and respiratory rate is 25/min. On examination, the child appears sick. He has cervical lymphadenopathy on the right and decreased range of motion of his neck. His voice is muffled and sounds hoarse. His oropharynx is erythematous and a bulge is noted in the posterior pharyngeal wall. A lateral radiograph of the neck is shown below. Which of the following is the most likely diagnosis?
Viral pharyngitis
Infectious mononucleosis
Diphtheria
Epiglottitis
Retropharyngeal abscess
A 20-year-old man presents to the infectious diseases department with a large 7 cm× 8 cm swollen painful lump in the left anterior triangle of his neck. He has night sweats, 10 kg weight loss and a dry cough for the last month. He was treated with surgery and radiotherapy for a high grade astrocytoma when he was 8 years old. Which of the following is not a recognized complication of his childhood condition and its treatment?
Educational difficulties
Finger clubbing
Haematological malignancy
Infertility
Short stature
A 6-year-old boy has multiple, honey-colored, crusted lesions on his face, periungual areas, and forearms. The first lesion appeared 2 weeks ago on his philtrum. Since then the lesions have spread to his hands and arms. Each began as a small pustule on an erythematous base and eventually ruptured to form the crusted lesions now present. His temperature is 100.6 F, pulse is 100/min, and respirations are 14/min. The remainder of the physical examination is unremarkable. Which of the following is the most appropriate treatment?
Clarithromycin
Vancomycin
Penicillin G
Dicloxacillin
Penicillin V
A 5-year-old is referred to paediatrics due to concerns initially raised by his school teacher that he is weak and clumsy. On examination he has wasting of his quadriceps and walks in a waddling gait. His blood creatine kinase is 1600 mmol/L (normal is 24–190). What is the most likely diagnosis?
Spinal muscular atrophy
Acute myositis
Malnutrition with failure to thrive
Neglect with failure to thrive
Muscular dystrophy
A 7-year-old girl is brought to the physician because of an exanthematous rash associated with malaise and headache for 2 days. On examination, the child shows a fiery red facial rash with a characteristic "slapped cheek" pattern and pallor around the mouth. There is no fever. In immunocompromised patients, the pathogen that causes this condition may result in which of the following manifestations?
Progressive multifocal leukoencephalopath (PML)
Non-Hodgkin lymphoma
Encephalitis
Aplastic anemia
Symmetric polyarthritis
A 17-year-old adolescent comes to your office seeking help for “heavy” menses. Your review of systems also reveals weekly epistaxis. Her only significant past history includes a tonsillectomy at age 6 after which she required blood transfusion for excessive bleeding. Her family history includes several people who seem to bleed and bruise more easily than others. The patient’s mother required a hysterectomy after child birth for excessive hemorrhage. You order a variety of laboratory tests. The patient has a hemoglobin of 6.5 mg/dL with an MCV of 60%; her platelet count is 350,000/µL. Her von Willebrand antigen and her von Willebrand factor (vWF) activity (ristocetin cofactor activity) are decreased. Her vWF is reported as normal but in decreased amounts. You have been unable to reach her to report the findings, but when she calls about 1 week later she reports she is having a mild to moderate nosebleed. You initiate therapy with which of the following?
Aminocaproic acid (Amicar)
vWF concentrate alone
Desmopressin (DDAVP)
VWF with factor VIII
Intravenous immunoglobulin (IVIG)

A 6-year-old boy is often teased at school because he has stooled in his underwear almost daily for the last 3 months. He was toilet trained at 2 years of age without difficulty, but over the last 2 years he had developed ongoing constipation. His family is frustrated because they cannot believe him when he says “I didn’t know I had to go.” He is otherwise normal; school is going well, and his home life is stable. His only finding on examination is significant for stool in the rectal vault. The plain radiograph of his abdomen is shown. Initial management of this problem should include which of the following?
Time-out when he stools in his underwear
Daily enemas for 4 weeks
Barium enema and rectal biopsy
Family counseling
Clear fecal impaction and short-term stool softener use
A 2-month-old baby is brought in by the babysitter because he has been crying since she arrived to look after him and his right leg looks swollen. He is the only child living in the household. She does not think he is moving it and is worried it is injured. On examination he is miserable, his heart rate is 160, respiratory rate of 56, and capillary refill is less than 2 seconds. He has a swollen right thigh. He cries more when that leg is examined. You note a yellow bruise on his left thigh and two purple bruises on either arm. X-rays show a fracture of the right femur but the arms appear intact. A chest x-ray shows three healing posterior rib fractures. You are highly suspicious of non-accidental injury. What is the most appropriate management?
Give analgesia and plaster the leg fracture. Call the police to bring the parents to hospital
Give analgesia and plaster the leg fracture. Ask the babysitter to bring him back with the parents because he needs to be admitted
Give analgesia. Call the duty social worker on-call to get permission to discharge him once his leg has been plastered
Give analgesia and plaster the leg fracture. Contact the parents and inform them that he needs to be admitted. Ask them to come to the hospital and inform social services once they have arrived and been updated
Give analgesia and plaster the leg fracture. Call the police to arrest the babysitter for child abuse
A 2-month-old female infant born at term is brought to the office for a well-baby visit. Her antenatal and birth histories are unremarkable. Her developmental milestones are all normal for her age. Ophthalmoscopic examination reveals a white reflex in the right eye. The rest of the examination is normal. What is the most appropriate next step in the management of this patient?
Covering the affected eye
Referral to an ophthalmologist
Reassurance
Covering the normal eye
Watchful waiting

A mother arrives to the clinic with her three children (ages 2 months, 18 months, and 36 months). The 18-month-old has an intensely pruritic scalp, especially in the occipital region, with 0.5-mm lesions noted at the base of hair shafts, as shown in the picture. Which of the following therapies should be avoided in this situation?
Advice to the mother that treatment will again be necessary in 7 to 10 days
Replacement of all commonly used brushes
Treatment of all household contacts with 1% lindane (Kwell)
Use of 1:1 vinegar-water rinse for hair for nit removal
Washing of all clothing and bedding in very hot water
You have been the primary practitioner for a 15-year-old girl since she was 3 years old. She never has been hospitalized, and her history, vital signs, and physical examination findings on this health supervision visit are normal. At each of the past two yearly visits, urinalysis revealed no abnormalities except 2+ protein. Her urinalysis today again reveals 2+ protein with no other abnormalities. Her complete blood count, measurements of serum electrolytes and serum complements, and antinuclear antibody test results are all normal. Two successive 24-hour urine collections reveal 321 and 387 mg protein. You now refer the girl to a pediatric nephrologist. Of the following, the MOST important next step for the pediatric nephrologist is to
Repeat the 24-hour urine collection
Obtain a first morning urine specimen
Repeat the urinalysis
Obtain renal ultrasonography
Perform a renal biopsy
The accident and emergency triage nurse asks you to look at a 3-year-old child with a short history of waking up this morning unwell with a cough and fever. She looks unwell, heart rate is 165, respiratory rate 56, saturations of 96 per cent in air, temperature of 39.3°C and central capillary refill of 4 seconds. She has a mild headache but no photophobia or neck stiffness and you notice a faint macular rash on her torso and wonder if one spot is non-blanching. You ask the triage nurse to move her to the resuscitation area and call your senior to review her. Fifteen minutes later your senior arrives and the spot you saw on the abdomen is now non-blanching and there is another spot on her knee. What are the three most important things to give her immediately?
High flow oxygen, IV fluid bolus, IV ceftriaxone
High flow oxygen, IV ceftriaxone, IV methylprednisolone
IV fluid bolus, IV ceftriaxone, IV fresh frozen plasma
High flow oxygen, IV ceftriaxone, IV fresh frozen plasma
IV fluid bolus, IV ceftriaxone, IV methylprednisolone
During the health supervision visit of a 2-year-old boy who is new to your practice, you note a productive cough that his mother says has been present for several months. His weight is below the 5th percentile. Fine crackles are present in his lungs bilaterally, and he has mild clubbing of the fingers. The remainder of his physical examination findings are unremarkable. A chest radiograph reveals poorly defined bronchovascular markings and a few cystic spaces bilaterally, prompting you to order computed tomography scan of the chest, which reveals diffuse bronchiectasis. Of the following, the MOST likely diagnosis is
Allergic bronchopulmonary aspergillosis
Cystic fibrosis
Mycobacterium tuberculosis infection
Primary ciliary dyskinesia
Foreign body aspiration
A 4-day-old infant is brought to the physician for an outpatient follow-up visit. The mother's pregnancy and delivery were uncomplicated. The infant weighed 3.4kg (7 .5 lb) and was 19 in (48.2 cm) long at birth. He did well in the newborn nursery and was discharged from the hospital on day 2 of life. Today his mother reports that he is exclusively breastfed, and nurses for 10 minutes every 3 hours. He has 3-4 wet diapers a day, and has not had a bowel movement for two days. On examination, he weighs 2.95 kg (6.5 lb) and is 19 in (48.2 cm) long. He appears jaundiced on the face and chest. The remainder of the physical examination is unremarkable. Laboratory values are shown below. Total bilirubin 15 mg/dl, direct bilirubin 1 mg/dl, Infant's blood type O positive, Mother's blood type A positive. Which of the following is the most likely cause of this infant's hyperbilirubinemia?
Breast milk jaundice
Biliary atresia
Galactosemia
Breastfeeding jaundice
ABO incompatibility
A 2-year-old child has had red, weeping, crusted lesions of the face, scalp, diaper area, and extremities since about age 2 months, with multiple periods of exacerbation and improvement. Attempts to remove potentially irritating substances have not modified the course of the rashes. The child is noted to be constantly scratching and rubbing involved areas. There is a strong family history of hay fever and asthma. Which of the following is the most likely diagnosis?
Lichen simplex chronicus
Atopic dermatitis
Cellulitis
Seborrheic dermatitis
Contact dermatitis
You are asked to evaluate an infant born vaginally 3 hours previously to a mother whose only pregnancy complication was poorly controlled gestational diabetes. The nursing staff noticed that the infant was breathing abnormally. On examination, you find that the infant is cyanotic, has irregular, labored breathing, and has decreased breath sounds on the right side. You also note decreased tone in the right arm. You provide oxygen and order a stat portable chest radiograph, which is normal. Which of the following studies is most likely to confirm your diagnosis?
Induced sputum culture
Nasal wash for viral culture
Chest ultrasound
Fiberoptic bronchoscopy
Chest CT
A 4196 g (9 lb 4 oz) infant is delivered via vaginal delivery to a 31-year-old mother with gestational diabetes. The delivery was complicated by shoulder dystocia. He is taken to the newborn nursery where his initial plasma glucose level is 20 mg/dL. The initial spun hematocrit is 65%. Which of the following congenital anomalies is this baby most likely to have?
Small left colon
Cleft palate
Aniridia
Omphalocele
Macroglossia
A 12-year-old girl presents to the emergency department with abdominal pain. Her parents report that she awakened with a temperature of 101°F (38.4°C) this morning, complained of abdominal pain, and has vomited twice. There is no diarrhea, and there are no sick contacts. She reports nausea and no interest in food or drink. She was previously entirely healthy. Urinalysis reveals a specific gravity of 1.015 and is otherwise normal. Of the following, the finding that MOST indicates the need for immediate surgical intervention is
Pain in the right lower quadrant
Hyperactive bowel sounds
Abdominal distention
Rigidity of the abdominal wall
Voluntary guarding
A previously healthy, active, 18-month-old African American child presents with unilateral nasal obstruction and foul-smelling discharge. The child’s examination is otherwise unremarkable. Which of the following is the most likely diagnosis?
Choanal atresia
Frontal sinusitis
Nasal polyps
Deviated septum
Foreign body
A 10-hour-old newborn is noted to have a swelling in the scalp which was not present at birth. The swelling is limited to the surface of one cranial bone. There are no visible pulsations, indentations of the skull, or discoloration of the overlying scalp. What is the most likely diagnosis?
Caput succedaneum
Cranial meningocele
Intracranial hemorrhage
Depressed skull fracture
Cephalohematoma
A 7-year-old boy presents with tenderness and erythema of one knee joint. He has had troubles with infections since about 3 months of age. A brother and a maternal uncle both died of infectious disease at an early age. A detailed immunologic evaluation performed at 2 years of age demonstrated plasma IgG less than 50 mg/100 mL. Normal numbers of circulating T cells and normal cellular immunity were found. The boy had been treated monthly since then with IV immunoglobulin. This therapy had markedly reduced, but not eliminated, the boy's infection rate. Which of the following is the most likely pathogen to cause infectious arthritis in this patient?
Aspergillus
Mycoplasma
Mycobacteria
Herpes
Toxoplasma
A 2-week-old baby was referred to the prolonged jaundice clinic by the community midwife. The pregnancy was unremarkable, and she was born at term with no antenatal abnormalities on ultrasound (US) scans or blood serology. She is now 17 days old and has been jaundiced since day 5 of life and never required phototherapy. She is breastfed and feeds 3-hourly for 20–25 minutes. She is afebrile and not lethargic. Her mother reports that the stools are pale and she has dark coloured urine. The bilirubin is 300 µmol/L, and conjugated bilirubin 100 µmol/L. What is the most important diagnosis to exclude?
Biliary atresia
Breast milk jaundice
Neonatal hepatitis
ABO incompatibility
Hypothyroidism
A 1-year-old African American infant is in for well-child care. He is primarily breast-fed. His parents do not give him much solid food because he has no teeth. He receives no medications or supplements. His parents are concerned about his bowed legs. On examination, you note some other bony abnormalities including frontal bossing, enlargement of the costochondral junctions, a protuberant sternum (pigeon chest), and severe bowing of the legs. You obtain x-rays to confirm your clinical diagnosis and also note a healing fracture of the left femur. Which of the following is the most likely diagnosis?
Osteogenesis imperfecta
Scurvy
Chondrodystrophy
Congenital syphilis
Rickets
A woman comes to an emergency department because she is in labor. She has had no prenatal care. Her baby is delivered and appears to be of about 32 weeks' gestation. The newborn is very pale and shows severe, generalized edema. Cord-blood hematocrit is 22%, and cord-blood bilirubin is 7 mg/dl. Ultrasound examination demonstrates pleural effusions, ascites, cardiomegaly, and hepatomegaly. Which of the following is the most likely diagnosis?
Beta thalassemia
Sickle cell anemia
ABO incompatibility
Congenital spherocytosis
Rh incompatibility
A 7 -year-old boy is brought to the emergency department after falling on his outstretched hand. On examination, there is minimal swelling at the right elbow. The skin on the right forearm appears tense, and severe pain is present. The brachial pulses are good bilaterally, and sensations are intact in both upper limbs. X-rays of the right upper limb show a displaced anterior fat pad. Which of the following statements is true about this condition?
Fracture of forearm bones is responsible for the swelling
Suspect child abuse and report the case to child protection services
The presence of brachial pulse on the right side rules out the possibility of vascular compromise
The treatment should consist of immediate cast placement
Forearm swelling is due to ischemia of the forearm soft tissues
A 16-year-old girl who was treated successfully for leukemia that presented as a mediastinal mass at 2 years of age comes to your office complaining of a "lump" in her neck of 3 weeks' duration. On physical examination, you note a firm, hard, fixed mass that seems to be part of the left lobe of the thyroid and scattered shotty lymphadenopathy on the left. Of the following, the MOST informative laboratory study for this patient is
131-iodine thyroid scan
Technetium thyroid scan
Serum calcitonin concentration
Thyroid ultrasonography
Fine-needle aspiration thyroid biopsy
Your 6-year-old son awakens at 1:00 AM screaming. You note that he is hyperventilating, is tachycardic, and has dilated pupils. He cannot be consoled, does not respond, and is unaware of his environment. After a few minutes, he returns to normal sleep. He recalls nothing the following morning. Which of the following is the most likely diagnosis?
Psychiatric disorder
Migraine headache
Night terrors
Seizure disorder
Drug ingestion
Numerous therapeutic agents are known to have teratogenic effects on the developing fetus. Of the following, the findings in the newborn that are MOST suggestive of prenatal exposure to an angiotensin-converting enzyme inhibitor are
Microtia and conotruncal malformation
Neonatal anuria and patent ductus arteriosus
Smooth philtrum and lip
Deafness and cataracts
Nasal hypoplasia and stippled epiphyses
An otherwise healthy 7-year-old girl is brought to your office by her father because she has some acne, breast development, and fine pubic hair. Which of the following is the most likely etiology for her condition?
Early onset of “normal” puberty (constitutional)
A lesion of the central nervous system (CNS)
A feminizing ovarian tumor
Exogenous estrogens
A gonadotropin-producing tumor
A school teacher calls you to report that his 7-year-old student had about 10 episodes of eye blinking and gabbling today, which lasted approximately 30 seconds each. The child sat in his chair and did not have any postictal confusion. The teacher noticed several similar episodes during the last month, as well as a decline in the child's school performance. What type of seizure does this child have?
Simple partial seizures
Complex partial seizures
Absence seizures
Generalized tonic-clonic seizures
Atonic seizures
You are examining a newborn infant in the well-baby nursery. The infant was the product of a benign pregnancy and vaginal delivery; he appears to be in no distress. Interestingly, your measurement of fronto- occipital head circumference is about 2 cm larger than the initial measurement done several hours before. Your examination otherwise is significant for tachycardia and a “squishy” feel to the entire scalp. You can elicit a fluid wave over the scalp. Management of this condition should include which of the following?
CT scan of the skull with bone windows
Elevation of the head of the crib
Observation and parental reassurance
Transfer to the newborn ICU
Surgical drainage
A one-day-old infant with Down syndrome has developed persistent vomiting. He was delivered vaginally at 34 weeks without any complications. On examination, he appears dehydrated and slightly tachypneic. His abdomen is soft and not distended. Abdominal x-ray reveals two large distinct air bubbles, but there are no dilated bowel loops or air fluid levels. What is the most likely diagnosis of this patient?
Reflux disorder
Tracheoesophageal fistula
Pyloric stenosis
Bowel obstruction
Duodenal atresia
A 3-year-old boy is brought by his father to the Emergency Department with fever, headache and neck pain that developed over the past several hours. The father states he is not the birth father, and that he and his wife adopted the boy at 18 months of age after his birth mother abandoned him. Physical examination reveals a lethargic male with a temperature of 39.7 C (103.5 F). There is photophobia, and mildly injected conjunctiva are appreciated. Pupils are equal and reactive and funduscopic examination is unremarkable. The patient has neck stiffness with a positive Kernig's sign. A complete blood count reveals a leukocyte count of 24,000/mm3 with 64 segmented neutrophils and 25 bands. A lumbar puncture is performed that reveals elevated CSF pressure, decreased glucose, and elevated protein. A Gram's stain shows gram-negative pleomorphic rods. There is no growth on blood agar. Growth on chocolate agar reveals white colonies. Which of the following is the most likely pathogen?
Listeria monocytogenes
Neisseria meningitidis
Haemophilus ducreyi
Streptococcus pneumoniae
Haemophilus influenzae type b

A 10-year-old patient (pictured below) calls his parents from summer camp to state that he has had fever, muscular pain (especially in the neck), headache, and malaise. He describes the area from the back of his mandible toward the mastoid space as being full and tender and that his earlobe on the affected side appears to be sticking upward and outward. Drinking sour liquids causes much pain in the affected area. When his father calls your office, you remind him that he had refused immunizations for his child on religious grounds. Which of the following preventable diseases has this child acquired?
Rubella
Varicella
Measles
Mumps
Diphtheria
A week-old infant presents blood in his stools. He was born at home, with the father assisting in the delivery; no physician or midwife was present. He has been breast-fed and has been nursing well. On examination, you also note some blood in his nose. He is not jaundiced; a rectal examination and guaic test of the stool confirms that blood is present. His examination is otherwise normal. He is on no medications. Which of the following is the most likely diagnosis?
Sepsis
Breast milk allergy
Liver disease
Vitamin K deficiency
Child abuse
A 9-year-old girl is stung on the left leg by a hornet while playing outside. Within 10 minutes, she experiences diffuse pruritus, and a large area of erythema develops at the sting site. Five minutes later, extensive raised welts appear on her trunk and extremities. Her parents rush her to the emergency department, where intravenous antihistamines and steroids are administered. During this episode, she denies difficulty breathing or swallowing. No tongue or uvula edema is evident during examination, and her symptoms gradually resolve over 4 hours. Of the following, the NEXT recommended step in her management is to
Admit the girl to the hospital for 24 hours
Start allergy shots to hornet
Prescribe a daily oral antihistamine for the girl to take when playing outside
Discharge the girl to home
Perform skin testing to hornet and other stinging insects within the next 72 hours
A 3-month-old boy is brought to the pediatrician because of a red growth on his arm. The pregnancy had been uncomplicated, and the infant has been meeting all development milestones. He has been healthy so far and has received all scheduled immunizations. He is currently being breast-fed. His skin was clear at birth, but when he was 2 months old, his mother noted a light red growth on his arm. Within the past month, it has increased in size and has turned bright red. Which of the following is the most appropriate treatment for this disorder?
Topical corticosteroids
Argon laser therapy
Surgery
Observation
Radiation therapy
A 7-year-old girl presents with hives, which developed after a bee sting. She has no other symptoms. The hives resolve with diphenhydramine. Which of the following is the most appropriate management?
Order a skin-prick test with hymenoptera venom
Admit to the hospital for observation for delayed hypersensitivity symptoms
Write a prescription for diphenhydramine in case she is bitten again
Refer her to an allergist for desensitization
Provide an Epi-pen Jr (epinephrine auto injector) to be carried at all times, as well as a prescription for diphenhydramine
A 9-year-old girl is seen in the office for unsteady gait and weakness in the lower limbs. On examination she is found to have a widebased gait with constant shifting of position to maintain her balance. There is decreased vibratory and position sense in the lower extremities, and ankle jerks are absent bilaterally. Her feet are deformed with high plantar arches. MRI of the brain and spinal cord shows marked atrophy of the cervical spinal cord and minimal cerebellar atrophy. Nerve conduction velocity results are within normal limits. EKG shows T-wave inversions in the inferior and lateral chest leads. The mother says that her other child, a 3-year-old boy, is completely normal. He shares toys with his sister and plays well with other children at playschool. He is able to copy squares and crosses but is unable to copy a triangle. Which of the following statements would you advance while discussing the girl's condition with her mother?
I advise you to go for prenatal counseling if you desire any future pregnancies
There is nothing to worry about since it's a non-progressive condition
It is most likely a result of spontaneous mutation & the chances of your boy developing the same condition are minimal
The inability of your boy to copy a triangle worries me since it may be an early manifestation of the same condition your daughter is suffering from
The EKG abnormalities are most likely due to myocardial ischaemia
A 9-year-old boy presents with a 3-month history of multiple episodes of sudden awakening at night. His mother states that when he wakes up suddenly, he screams, "Go! Get away! Go!" and does not respond to the parents. His eyes are wide open, and he sweats heavily and looks scared. The parents have had to struggle to awaken him. After the episodes, he has no memory of what happened. Which of the following is the most likely diagnosis?
Obstructive sleep apnea
Panic disorder
Night terrors
Nightmares
Confusional arousals
A 4-year-old boy presents to your clinic for a second opinion. He has a 3-week history of diarrhea, abdominal pain, and tenesmus. The parents state that he seems to be getting worse, and nobody has been able to help them despite "a bunch of tests on his poop." His stool output has increased from four to five per day to eight to ten per day during the past week, and he now has a temperature of 102°F (38.9°C). They are starting to see what appears to be blood in the toilet after he goes to the bathroom. According to the parents, the boy was in good health until 1 week after they returned from a fishing trip on the Amazon river. Physical examination reveals a moderately illappearing boy who has diffuse abdominal pain. During your examination, he passes a very foul-smelling stool that appears to be a mixture of blood and pus, which you send to the laboratory for analysis. Of the following, the MOST appropriate next test is
Colonic biopsy
Barium enema
Gallium scan
Abdominal ultrasonography
Liver function test
A 6-year-old boy is brought to the office by his parents after hearing that chicken pox is infectious and can occur in unimmunized contacts. One week ago, he and his family visited relatives, and one of his cousins had chicken pox at that time. He and his two other siblings are apparently healthy, and never had any "chicken pox shots." What is the best next step in the management of this patient?
Tell the parents that the patient might develop a rash within the next two weeks
Administer varicella vaccine to the patient
Give intravenous immunoglobulins to the patient
Administer varicella vaccine and intravenous immunoglobulins to the patient
Administer acyclovir to the patient
A routine prenatal ultrasound reveals a male fetus with meningomyelocele. The 24-year-old primigravid mother is told the infant will require surgery shortly after birth. You counsel her about the etiology of this defect and the risk of further pregnancies being similarly affected, and state which of the following?
Supplementation of maternal diet with folate leads to a decrease in incidence of this condition
The hereditary pattern for this condition is autosomal recessive
The prenatal diagnosis can be made by the detection of very low levels of alpha- fetoprotein in the amniotic fluid
Neither environmental nor social factors have been shown to influence the incidence
Subsequent pregnancies are not at increased risk compared to the general population
A 3 year old is brought into accident and emergency by ambulance following a generalized tonic clonic seizure that lasted 2 minutes. She did not require any treatment to stop the seizure but on arrival the ambulance crew measured her temperature as 39.2 °C and gave paracetamol. She is now apyrexial with a heart rate of 140, respiratory rate of 30 and capillary refill less than 2 seconds. On examination she has red enlarged tonsils with no pus, no neck stiffness or rash. What is the most appropriate management?
Discharge home with rescue buccal midazolam for future seizures
Start phenytoin
Oral penicillin
Explain that this was a febrile convulsion and discharge home
Lumbar puncture and IV ceftriaxone
A 3 month old is brought into accident and emergency with a generalized tonic clonic seizure. She is apyrexial and the seizure stopped after 15 minutes with rectal diazepam given by the ambulance crew. Her heart rate is 130, respiratory rate of 36 and capillary refill is less than 2 seconds. On examination she is drowsy, has a port wine stain on her forehead but is otherwise normal on examination. What is the most likely cause of her seizure?
Meningitis
Sturge–Weber syndrome
Tuberous sclerosis
Neurofibromatosis type II
Neurofibromatosis type I
The parents of a 10-year-old girl with newly diagnosed, generalized tonic-clonic epilepsy come to the physician seeking advice regarding what they should do when the child has a seizure. Which of the following suggestions is appropriate?
Try to restrain the child during the seizure
Put something in the child's mouth at the onset of seizure
Do not allow the child to return to her activities after recovery
Call an ambulance immediately as soon as seizure begins
Try to place the child on her side during the seizure
A 4-year-old girl remains intubated, mechanically ventilated, and completely unresponsive in the intensive care unit following a massive subarachnoid hemorrhage of unknown cause. She is hemodynamically stable and not receiving any sedating medications. She has a temperature of 98.1ºF (36.7ºC) and has no evidence of infection. The girl has not exhibited any brainstem or cerebral function for more than 24 hours. Of the following, the statement you are MOST likely to make while on rounds with the resident team is that
A nuclear medicine blood flow study is the best method to determine whether the girl is brain dead
Electroencephalography must be performed to ascertain whether this girl is dead
Even though this child is brain dead, her stable cardiac status precludes a declaration of death
Organ donation is contraindicated in this child once she is declared dead
No further testing is indicated because this child is brain dead
A new mother complains that her 6-week-old infant frequently regurgitates small volumes of formula during and after feedings. Physical examination demonstrates a happy baby who has gained half a pound since his last visit. No abdominal masses are noted. Which of the following is the best next step in management?
Monitor the baby carefully
Order CT of the abdomen
Change the bottle's nipple
Order abdominal x-rays
Change the baby's formula
A 12-year-old boy is brought to the emergency department with a temperature of 39.1 C (102.4 F) at home, difficulty speaking, and odynophagia for 2 days, Physical examination reveals marked erythema of the right tonsil pillar and edema of the uvula with deviation to the left. In addition to anaerobic bacteria, which of the following organisms is most likely to be isolated from a tonsillar pillar aspirate?
Streptococcus pneumonia
Haemophilus influenzae type b
Beta-hemolytic Streptococcus
Enterococcus
Staphylococcus aureus
A 4-year-old child has been losing weight recently and has been vomiting for the past 24 hours, unable to eat anything. His mother has brought him into accident and emergency out of concern as he seems confused. The triage nurse has taken him to the resuscitation room and asked for your help. On examination he is drowsy, has a heart rate of 150, respiratory rate of 60 and a central capillary refill of 5 seconds. He has subcostal recessions and good air entry bilaterally with no added sounds. He moans when you examine his abdomen but there are no masses. You put in a canula and take bloods. The venous blood gas shows: pH 7.12, PCO2 2.3 kPa, PO2 6.7 kPa, HCO3– 15.3 mmol/L, BE –8.6, Glucose 32.4 mmol/L. What is the most likely diagnosis and what is the first management step?
Gastroenteritis with severe dehydration, give a fluid bolus
Diabetic ketoacidosis, start an insulin infusion
Diabetic ketoacidosis, give a fluid bolus
Pneumonia, start IV co-amoxiclav
Ruptured appendix, give a fluid bolus and book the emergency operating theatre
You are called to examine a one-day-old male neonate who gradually developed cyanosis over the past few hours. The infant was delivered vaginally at full term, assisted with forceps, and weighed 9 lbs. The Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Oxygen administration by mask does not relieve the cyanosis. Further examination reveals tachypnea, subcostal retractions, a normal S 1, single and loud S2, and no murmur. Which of the following is the most probable cause of the infant's cyanosis?
Coarctation of aorta
Atrial septal defect
Transposition of great vessels
Ventricular septal defect
Patent ductus arteriosus
A 12-year-old basketball player has complained of right knee pain immediately after games for 2 weeks. Although he had complained of knee pain intermittently earlier in the season, there is no history of swelling or injury of the knee. Physical examination findings of the knee are remarkable for full range of motion no effusion, and swelling over the proximal right tibia that is tender to palpation. Of the following, the MOST likely diagnosis is
Sinding-Larsen Johansson disease
Osgood-Schlatter disease
Patellofemoral syndrome
Jumper's knee
Prepatellar bursitis
A 3-year-old boy who has spina bifida has a history of recurrent urinary tract infections (UTIs). He is currently being treated for a UTI. Monitoring laboratory evaluation shows a blood urea nitrogen of 23 mg/dL (8.2 mmol/L) and a creatinine concentration of 1.1 mg/dL (97.2 mcmol/L). Of the following, the class of antibiotics that is MOST commonly associated with renal toxicity is
Azalides
Aminoglycosides
Carbapenems
Penicillins
Cephalosporins
A 9-year-old boy is brought to the pediatric clinic by his mother, who noticed that the left side of his mouth has started to droop over the past several days. In addition, he is unable to close his left eye completely and complains of it burning. Review of systems reveals a cold approximately two weeks ago and recent decreased taste sensation. Physical examination reveals a well-nourished male with normal vital signs. There is left eye ptosis and mild erythema of the left conjunctiva. His smile is asymmetrical on the left. Laboratory evaluation, including a complete blood count and chemistry profile, are normal. Which of the following infections is most closely associated with this patient's condition?
Measles
Influenza
Epstein-Barr Virus
Group A Streptococcus
Human Immunodeficiency Virus
A 3-year-old child who has a history of recurrent otitis media with effusion (OME) in infancy is brought to the clinic. His mother is afraid that he has a hearing loss because he does not talk as much as his brother did at the same age. He speaks in three-word sentences, and you can understand fewer than 50% of his words. Results of his physical examination, including the ears, are normal. Of the following, the MOST appropriate statement regarding this child's condition is that:
Even mild conductive hearing loss could affect his later school performance without frank speech delay
Performing hearing screening solely in response to parental concern is not recommended
Testing air and bone conduction thresholds in the office will help you rule out hearing loss
OME does not cause conductive hearing loss severe enough to cause speech delay
The absence of middle ear fluid rules out conductive hearing loss
A 7-year-old boy who has had pain in his right leg for 4 months is being evaluated. The pain is worse at night and is unrelenting, but it can usually be relieved with ibuprofen. On physical examination, there is localized tenderness over the anterior aspect of the right thigh. There is also mild atrophy of the affected limb. A radiograph of the femur reveals a radiolucent nidus with surrounding reactive sclerotic bone. Which of the following is the most likely diagnosis?
Osteoid osteoma
Ewing sarcoma
Brodie's abscess
Stress fracture
Osteosarcoma
A 7-year-old boy has a history of repeated urinary tract infections that have been treated by the empiric use of antibiotics. The parents are not satisfied with the care the child is receiving, and they take him to a pediatric urologist. Evaluation by voiding cystourethrogram shows that the patient has vesicoureteral reflux without ureteral or upper tract dilatation (grade one reflux). Which of the following is the appropriate management for this child?
Surgical reimplantation of the ureter
Nephrectomy on the affected site
Long-term, low-dose antibacterial therapy
Alpha blockers
Reassurance and observation
A 5-year-old girl is being evaluated for generalized swelling. Her blood pressure is 98/60 mm Hg. Her laboratory results show: Creatinine 0.7 mg/dl, Albumin 1.6 g/dL, Cholesterol 360 mg/dL, Triglycerides 400 mg/dL, C3 complement 120 mg/dL (normal, >80 mg/dL), Antinuclear antibody Negative, Urinalysis 1 RBC/hpf, protein 400 mg/dL. Which of the following is the most likely diagnosis?
Membranoproliferative glomerulonephritis
Minimal change disease
Systemic lupus erythematosus
Membranous glomerulopathy
Postinfectious acute glomerulonephritis
A 1-week-old black infant presents to you for the first time with a large, fairly well-defined, purple lesion over the buttocks bilaterally, as shown in the photograph. The lesion is not palpable, and it is not warm nor tender. The mother denies trauma and reports that the lesion has been present since birth. This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. Which of the following is the most appropriate course of action in this infant?
Report the family to child protective services
Reassurance of the normalcy of the condition
Administration of vitamin K
Soft tissues films of the buttocks to identify calcifications
Measurement of bleeding time as well as factor VII and XI levels
As part of your clinic responsibilities, you supervise allergy shots for patients who have allergic rhinitis. The nurse calls you about a 12- year-old girl who received her allergy shot 30 minutes ago and now is experiencing warmth and erythema over the injection site. On physical examination, the patient appears healthy and in no distress. Vital signs include a temperature of97.5°F (36.4°C), heart rate of 90 beats/min, and respiratory rate of 18 breaths/min. At the injection site, there is a 4 x 4 cm raised, erythematous, warm area. There is no edema of the tongue or uvula, and findings on her pulmonary, cardiovascular, and skin examinations are otherwise normal. Of the following, the NEXT most appropriate action is to
Allow the patient to leave the clinic
Observe the patient for an additional 30 minutes
Administer an oral antibiotic
Administer intramuscular epinephrine
Discontinue allergy shots
A baby is born to a mother who is positive for hepatitis B surface antigen (HBsAg). Your plan is to do which of the following?
Give the infant a hepatitis B immunization
Give the infant hepatitis B immune globulin (HBIG)
Obtain liver function tests and hepatitis serology of the infant
Give the HBIG only if the child is positive for HBsAg
Give the infant a hepatitis B immunization and HBIG
A vomiting infant is brought to the emergency room. The blood work results reveal a normal blood count, but a hyponatremic, hypochloremic, metabolic alkalosis. Which of the following would be consistent with these findings?
Ethanol poisoning
Isoniazid ingestion
Cystic fibrosis
Diabetes mellitus
Iron ingestion
A 12-hour-old baby on the post-natal ward has just had a seizure lasting 2 minutes. It resolved spontaneously and was generalized in nature. Her mother had gestational diabetes and poor glucose control in pregnancy. The baby’s birth weight was 5 kg. There were no abnormalities noted on antenatal US scans or maternal serology. On examination she has no dysmorphic features and handles well. What initial blood tests would you do for the baby?
Calcium, magnesium
Liver function tests
Electrolytes
Boehringer Mannheim (BM) glucose
Full blood count, C-reactive protein
A 21-year-old woman has just delivered a term infant. She has had only one visit to her obstetrician, and that was at about 6 weeks of pregnancy. She provides her laboratory results from that visit. The delivered infant is microcephalic, has cataracts, a heart murmur, and hepatosplenomegaly. Your further evaluation of the child demonstrates thrombocytopenia, mild hemolytic anemia, and, on the echocardiogram, patent ductus arteriosus and peripheral pulmonary artery stenosis. Which of the following maternal laboratory tests done at 6 weeks gestation is likely to explain the findings in this child?
Negative triple screen
Positive rapid plasma reagin (RPR) with negative Micro hemagglutination Treponema pallidum test(MHATP)
Negative rubella titer
Positive varicella titer
Positive hepatitis B surface antibody
A 6-year-old boy with a history of asthma and eczema is brought in to accident and emergency from a local restaurant. He is on high flow facial oxygen with significant facial oedema and generalized erythema. On auscultation there is widespread wheeze for which the ambulance crew gave a salbutamol nebulizer. What is the next step in management?
Insert an IV line and give 200 µg of 1:10 000 intravenous adrenaline
Insert an IV line and give 10 mg slow intravenous antihistamine
Give intramuscular 1:1000 adrenaline, 250 µg
Insert an IV line and give 100 mg slow intravenous hydrocortisone
Repeat the salbutamol nebulizer and call for an anesthetist for intubation
A 1-month-old baby attends accident and emergency with a 2-day history of fever to 38.8°C measured at the GP surgery. He has been vomiting, with no diarrhoea, rash, cough or coryza. A clean catch urine has leukocytes +++ and ketones, no nitrites, blood or protein. An urgent microscopy shows >200 cells/ µL white cells. What is the most appropriate course of action?
Organize an urgent DMSA scan
Admit for a course of IV antibiotics to cover a urinary tract infection (UTI)
Admit for a lumbar puncture, blood cultures and chest x-ray, IV antibiotics
Discharge home with reassurance and advice to return if fever persists
Discharge home with 3 days of trimethoprim
A 9-month-old boy is taken to the emergency room because of high fever. Breath sounds are diminished in the lungs, and a chest x-ray film shows lobar pneumonia. Probable streptococcal pneumonia is demonstrated in Gram's stain of sputum and then later confirmed by culture. The child responds to antibiotic therapy. A detailed history is taken during the admission, which reveals that this is the third episode of pneumonia in this young child; the two previous episodes occurred at 6 and 7.5 months of age. One of the mother's brothers had died of infection at age 9. Immunoglobulin studies demonstrate the following: IgG 80 mg/dL [normal 723-1685 mg/dL], IgA 60 mg/dL [normal 81-463 mg/dL], IgM 20 mg/dL [normal 48-271 mg/dL]. Studies of the lymphocyte population demonstrate normal numbers of T cells and markedly decreased B cells. Which of the following is the most likely diagnosis?
Transient hypogammaglobulinemia of infancy
Common variable immunodeficiency
Wiskott-Aldrich syndrome
DiGeorge syndrome
Bruton agammaglobulinemia
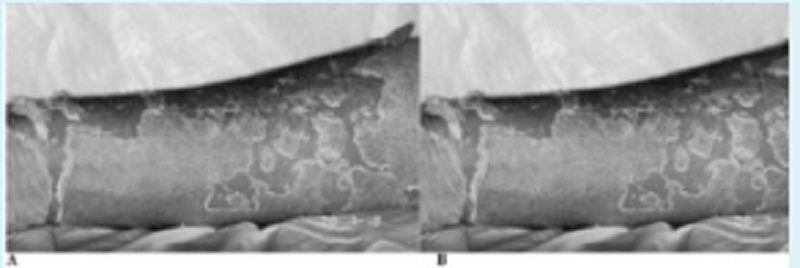
A previously healthy 4-year-old child pictured below presents to the emergency room (ER) with a 2-day history of a brightly erythematous rash and temperature of 40°C (104°F). The exquisitely tender, generalized rash is worse in the flexural and perioral areas. The child is admitted and over the next day develops crusting and fissuring around the eyes, mouth, and nose. The desquamation of skin shown in the photograph occurs with gentle traction. Which of the following is the most likely diagnosis?
Erythema multiforme
Scarlet fever
Staphylococcal scalded skin syndrome
Drug eruption
Epidermolysis bullosa
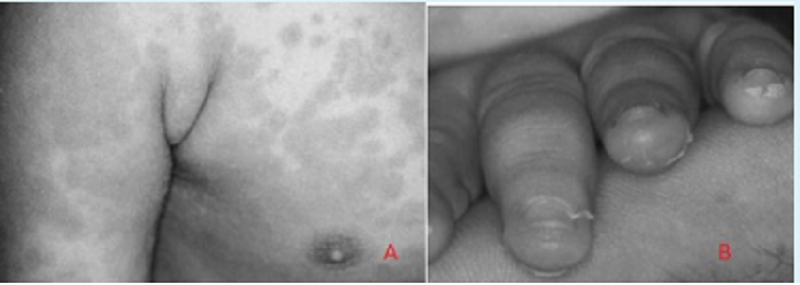
A 2-year-old boy is brought into the emergency room with a complaint of fever for 6 days and the development of a limp. On examination, he is found to have an erythematous macular exanthem over his body as shown in (image A), ocular conjunctivitis, dry and cracked lips, a red throat, and cervical lymphadenopa- thy. There is a grade 2/6 vibratory systolic ejection murmur at the lower left sternal border. A white blood cell (WBC) count and differential show predominant neutrophils with increased platelets on smear. Later, he develops the findings as seen in (image B). Which of the following is the most likely diagnosis?
Infectious mononucleosis
Kawasaki disease
Juvenile rheumatoid arthritis
Scarlet fever
Rheumatic fever
A 5-year-old boy presents to the emergency department with 2-day history of fever, anorexia, loose stools, and yellow skin color. He attends a large daycare center. On physical examination, his temperature is 38.1 C (100.7 F), blood pressure is 88/56 mm Hg, pulse is 74/min, and respirations are 15/min. Initial laboratory evaluation reveals a total bilirubin of 1.8 mg/dL and alanine aminotransferase of 764 U/L. Which of the following is the most appropriate diagnostic test?
IgG for hepatitis B surface antigen in serum
IgG for hepatitis A in serum
Stool culture for hepatitis A
IgM for hepatitis A in serum
Hepatitis B surface antigen in serum
An otherwise healthy 5-year-old boy is brought to the emergency department of a small hospital because of a simple 3-cm laceration in his forehead. The patient is crying and frightened. The practitioner decides to perform conscious sedation before suturing the laceration. Support personnel and equipment are available for monitoring the patient's vital status and carrying out resuscitation measures if needed. Which of the following is the most appropriate pharmacologic agent to achieve a safe level of conscious sedation in this situation?
Oral or rectal midazolam or diazepam
Concomitant analgesic-sedative agents and muscle relaxants
Intravenous propofol
Intravenous ketamine
Concomitant opioid and benzodiazepine administration
You are asked to see a 14-year-old girl who developed pubic hair at age 11 years and breast buds at age 12 years, but has not reached menarche. She is a gymnast who practices 2 hours a day. Breast tissue is Sexual Maturity Rating (SMR) 2 and pubic hair is SMR 4. She is 57 in tall and weighs 86 lb. The results of gonadotropin laboratory studies are a luteinizing hormone concentration of 18 mIU/mL (18 IU/L) (normal adult female, 2 to 70 mIU/mL [2 to 70 IU/L]) and a follicle-stimulating hormone concentration of 40 mIU/mL (40 IU/L) (normal adult female, 1 to 30 mIU/mL [1 to 30 IU/L]). Of the following, the MOST likely cause of the primary amenorrhea in this patient is
Excessive exercise
Prolactinoma
Autoimmune ovarian failure
Imperforate hymen
Turner syndrome
A 6-year-old girl has presented to her GP with a rapid increase in growth. Her mother is also concerned that she seems to have developed pubic and axillary hair and breast development prior to this but thought it would go away. She has no history of trauma and has reported problems with her vision. Her levels of gonadotrophin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH) and oestrogen are high. You are concerned that she may have a pituitary tumour. What is the likely visual field defect?
Monocular blindness
Bitemporal hemianopia
Myopia
Homonymous hemianopia
Central scotoma
A very concerned mother brings a 2-year-old child to your office because of two episodes of a brief, shrill cry followed by a prolonged expiration and apnea. You have been following this child in your practice since birth and know the child to be a product of a normal pregnancy and delivery, to be growing and developing normally, and to have no chronic medical problems. The first episode occurred immediately after the mother refused to give the child some juice; the child became cyanotic, unconscious, and had generalized clonic jerks. A few moments later the child awakened and had no residual effects. The most recent episode (identical in nature) occurred at the grocery store when the child’s father refused to purchase a toy for her. Your physical examination reveals a delightful child without unexpected physical examination findings. Which of the following is the most likely diagnosis?
Hyperactivity with attention deficit
Seizure disorder
Breath-holding spell
Drug ingestion
Pervasive development disorder
The mother and father of a newborn come in for the 2-week check-up. The mother complains of “colic” and asks if she can switch to goat’s milk instead of breast milk. Which of the following should be your main concern about using goat’s milk instead of breast milk or cow’s milk?
It has insufficient casein
It has insufficient calories
It has insufficient whey
It has insufficient fat
It has insufficient folate
A 2-day-old male infant presents with multiple episodes of bilious vomiting over the past 24 hours. He has a prominent tongue, flat occiput and slanting eyes. His hands are short, and there are wide gaps between his first and second digits. His abdomen is soft and without any distention, guarding or rigidity. On auscultation of the chest, there is a systolic ejection murmur along the left sternal border, with a wide and fixed splitting of S2. Abdominal x- rays show air trapped in the first portion of the duodenum and stomach. What is the most likely cause of the child's symptoms?
Mesenteric adenitis
Duodenal atresia
Pyloric stenosis
Acute appendicitis
Gastroesophageal reflux
A 24-month-old child is seen in the pediatrician's office for a regular health supervision visit. He has no history of developmental delay. He was born by an uncomplicated normal vaginal delivery at term, and he has not had any significant illness or injury prior to this visit. Which of the following motor milestones is most consistent with his age?
Copying a circle
Walking backward
Throwing a ball overhead
Building a tower of two cubes
Scribbling
A 6-day-old female neonate is admitted to the hospital for the evaluation of jaundice. She was born to a 17-year-old German mother at 39 weeks gestation. Her mother's blood type is B+, and was treated for newborn jaundice due to presumed ABO incompatibility. Her other family members also had neonatal jaundice. The infant's vital signs are normal. On examination, she is visibly jaundiced, and her spleen tip is palpable. Her total bilirubin level is 25mg/dl and direct bilirubin level is 0.4mg/dl. Her hemoglobin was initially 15.7g/dl, but is now 10.7g/dl. Her reticulocyte count is 4% and platelet count is 230,000/mm3. The peripheral smear shows moderate schistocytes with burr cells and moderate spherocytes. Her blood type is B+ and Coombs' test is negative. Her stools are negative for occult blood. Her mother's incubated red cell osmotic fragility study is abnormal. What is the most likely cause of this neonate's symptoms?
Isoimmune hemolytic disease of the newborn, due to ABO incompatibility
Hereditary spherocytosis
Autoimmune hemolytic anemia due to warm antibodies
Normal physiologic changes occurring in red cells in the neonatal period
Hereditary elliptocytosis
A 7-year-old child is scheduled for an elective tonsillectomy. The most important instruction to the parents should be to make sure that the child does which of the following?
Avoids contact with other children
Discontinues antibiotics 72 hour before surgery
Eats iron-laden foods for 3 weeks before surgery
Avoids aspirin and antihistamines for 2 weeks before surgery
Does not drink from siblings’ cups
A 16-year-old girl presents with lower abdominal pain and fever. On physical examination, a tender adnexal mass is felt. Further questioning in private reveals the following: she has a new sexual partner; her periods are irregular; she has a vaginal discharge. Which of the following is the most likely diagnosis?
Ovarian cyst
Appendiceal abscess
Ectopic pregnancy
Renal cyst
Tubo-ovarian abscess
Friends are considering adopting a “special needs” child from another country. The family has few details, but the information they have received so far suggests the 4-year-old child has had surgery for an endocardial cushion defect, is short for his age, and had a history of what sounds like surgically repaired duodenal atresia at birth. You are suspicious this child may have which of the following syndromes?
Kleinfelter
Waardenberg
Down
Turner
Marfan
You are admitting to the hospital a 3-month-old infant who has been having poor feeding, emesis, and diarrhea for 3 days. In the emergency center, her electrolytes were found to be: sodium 157 mEq/L, potassium 2.6 mEq/L, chloride120 mEq/L, bicarbonate 14 mEq/L,creatinine1.8 mEq/L, blood urea nitrogen(BUN) 68 mEq/L, and glucose195 mEq/L. She was given a fluid bolus in the emergency center and has subsequently produced urine. Which of the following is the most appropriate next step in her management?
Urinary electrolytes
Rehydration with free water
Slow rehydration over 48 hours
Continued rapid volume expansion with 1/4 normal saline
Packed red blood cells (RBCs)
You are called to see a hospitalized 9-year-old girl who suddenly has become dystonic, with her neck hyperextended, and is unable to move her eyes, now superiorly deviated. The nurses relate that this girl has non-Hodgkin lymphoma and has been receiving highly emetogenic chemotherapy. Of the following, the drug MOST likely to have caused this girl's symptoms and signs is
Aprepitant
Ondansetron
Diphenhydramine
Lorazepam
Metoclopramide
A newborn infant is brought to the nursery for evaluation after delivery. The mother reports that the pregnancy was uncomplicated, but she had only two prenatal visits. The infant was born via normal spontaneous vaginal delivery and required no resuscitation. The infant has hepatosplenomegaly on examination. While in the hospital, the infant requires treatment for anemia and hyperbilirubinemia. On subsequent examinations, the infant has clear rhinorrhea and ulcerative lesions on his feet. Which of the following congenital infections is most likely in this patient?
Syphilis
Rubella
Toxoplasmosis
Human immunodeficiency virus infection
Cytomegalovirus infection
A 3 year old male has sudden onset of dry cough with a small amount of bright red blood produced when he coughs. He has had no fevers, runny nose, or vomiting. In the Emergency Department a chest x-ray shows hyperexpansion of the right lung and clear lung fields. Which of the following is the most likely etiology of this child's symptoms?
Tuberculosis
Pulmonary arteriovenous malformation
Bacterial pneumonia
Foreign body aspiration
Cystic fibrosis
A 12-year-old child is struck in the right eye by a baseball. He now complains of double vision when he looks to the left. On physical examination, you note marked swelling and bruising circumferentially around the boy's right eye. His pupillary reflexes are normal, he has no blood in the anterior chamber of the eye, and his optic disc margins are sharp. He has dysconjugate gaze to the left but not to the right. His vision is 20/20 out of the left eye and 20/30 out of the right eye. Other findings on his neurologic examination are normal. Of the following, the MOST likely diagnosis is
Hyphema
Blow-out fracture
Corneal abrasion
Detached retina
Traumatic iritis
A 6-year-old girl presents with a 1-year history of periumbilical, nonradiating abdominal pain. The pain occurs at least three times per week and lasts up to 30 minutes. There is no history of heartburn, constipation, or diarrhea. Physical examination, complete blood count, erythrocyte sedimentation rate, and urinalysis yield normal results. A Helicobacter pylori serology (immunoglobulin G antibody) is positive. Of the following, a TRUE statement regarding this patient is that:
Empiric therapy with omeprazole and trimethoprim-sulfamethoxazole should be instituted
The positive serology should be confirmed by another diagnostic test
The H pylori antibody test is more sensitive in younger children than older children
This patient most likely has a gastric ulcer
The prevalence of H pylori increases with higher socioeconomic status
A 2-year-old boy who emigrated from Eastern Europe 1 year ago is brought to the physician because of fever, cough, and night sweats for 3 weeks. The child's grandmother, who lives with him, has similar symptoms. The child's temperature is 39.2 C (102.6 F), Wood pressure is 110/65 mm Hg, pulse is 90/min, and respirations are 28/min. A Mantoux test is reactive, and a chest x-ray film shows a right middle lobe infiltrate and hilar lymphadenopathy. Which of the following is the most appropriate next step in diagnosis?
Sputum induction
Gastric aspiration
Gastroscopy
Cervical lymph node biopsy
Pleurocentesis
A 17-year-old girl presents with amenorrhea of 6 months' duration. One year ago she joined the cross country team at school. At that time, her periods had been regular, about every 26 days, and remained so for the 3-month running season. At the end of the season, she continued to run 5 miles a day to be more competitive for the subsequent season. She noticed that her menstrual flow was lighter for a few months preceding the amenorrhea. You suspect exercise-induced amenorrhea and recommend a decrease in exercise. Of the following, the factor MOST likely to be associated with a low bone density and stress fractures in this patient is
High body mass index
Early onset of puberty
Cigarette smoking
Use of antidepressant medication
Use of oral contraceptives
A 5-month-old boy is brought to the office for a mass in his left groin area. The infant is on the examination table, quietly sucking on his pacifier. On examination, there is a fluid-filled sac that does not reach the inguinal ring and transilluminates well. Which of the following is the most likely diagnosis?
Inguinal hernia
Testicular tumor
Hematoma
Testicular torsion
Hydrocele
A premature neonate with respiratory distress syndrome is maintained on mechanical ventilation in a neonatal intensive care unit. Two weeks after delivery, the nurses in the intensive care unit notice that higher ventilation settings are needed and that more secretions are being suctioned from the endotracheal tube. A chest x-ray film shows questionable new infiltrates. Which of the following is the most likely pathogen?
Coagulase-negative oxacjllin-sensitive Staphylococcus
Methkillin-resistant Staphylococcus aureus
Group B Streptococcus
Methicillin-sensitive Staphylococcus aureus
Coagulase-negative oxacillin-resistant Staphylococcus
You are evaluating a 13-year-old boy who has a body mass index of 32 kg/m2 and a blood pressure of 140/80 mm Hg. Initial laboratory studies reveal fasting serum triglyceride levels of 180 mg/dL (2.0 mmol/L) (normal, 40 to 100 mg/dL [0.45 to 1.1 mmol/L]). You diagnose metabolic syndrome. Of the following, the MOST appropriate evaluation in addition to fasting blood glucose is
Serum alpha-fetoprotein
5-hour oral glucose tolerance test
Liver transaminases
Holter monitoring
Erythrocyte sedimentation rate
A 3-month-boy who has been previously healthy is brought to the emergency department with a 3-day history of rhinorrhea, mild cough, and wheezing. He has been afebrile and has had some difficulty feeding. His pulse oximetry reading is 90% on room air, respiratory rate is 60 breaths/min, and heart rate is 130 beats/min. Chest examination reveals mild subcostal retractions, scattered wheezes, and coarse crackles bilaterally. The rest of the physical examination findings are normal. Of the following, the pathogen that is MOST likely responsible for his symptoms is
Respiratory syncytial virus
Streptococcus pneumonia
Chlamydia trachomatis
Adenovirus
Haemophilus influenzae
A 42-year-old primigravida is in her 16th week of pregnancy. She is concerned about the possibility of her child having myelomeningocele. Of the following, the MOST useful diagnostic evaluation is
Fetal ultrasonography
Amniocentesis
Cordocentesis
Maternal alpha-fetoprotein screening
Chorionic villus sampling
A newborn female has loose neck skin and nonpitting edema of the lower extremities. Of the following, the MOST appropriate evaluation for this infant is
Blood chromosome analysis
Voiding cystourethrography
Magnetic resonance imaging of the brain
Ultrasonography of the liver
Slitlamp ophthalmologic examination
A 4-year-old boy, who has a ventriculoperitoneal shunt for congenital hydrocephalus, develops fever, headache, irritability, lethargy, photophobia, and vomiting. His temperature is 39.6 C (103.2 F). He is noted to have nuchal rigidity, with the presence of both Kernig's and Brudzinski's signs. The shunt tract is erythematous on the surface. A lumbar puncture is performed and shows a WBC of 40,000/mm3 with 85% neutrophils, a glucose concentration of 48 mg/dL, and a protein concentration of 169 mg/dL. Which of the following is the most likely pathogen?
Haemophilus influenzae
Staphylococcus epidermidis
Pseudomonas aeruginosa
Neisseria meningitidis
Streptococcus pneumoniae
An 11-month-old boy is brought to the emergency department by his parents. The child has a fracture of the right femur. The father reports this was sustained as a result of falling out of the crib. The child is also noted to have bruises on his shoulders and back. The rest of his examination is unremarkable. Which of the following is the most appropriate next step in diagnosis?
Lumbar puncture
Social services consult
Chest x-ray
CT of the head
Funduscopic exam
An 8-year-old boy presents to the pediatrician's office with a headache for the past 3 weeks. His mother also states that he has been more tired and has had frequent nose bleeding for the past month. On physical examination, his height and weight are both below the 5th percentile for his age. His blood pressure is 152/86 mm Hg in all four extremities. His pulse is 74/min, and respirations are 16/min. His heart examination is normal with no murmur. His peripheral pulses are strong and symmetric. Urinalysis and serum electrolytes are ordered. Which of the following is the most appropriate next step in diagnosis?
Serum Cortisol level
24-hour urine creatinine and protein
Plasma and urine catecholamine levels
Serum aldosterone leve
Blood urea nitrogen and creatinine concentration
A 3-year-old girl is brought to the emergency department because she became partially unconscious, lethargic and febrile. Her mother claims that "she suddenly took a turn for the worse" 24 hours ago after an upper respiratory tract infection. She has no allergies, and was not taking oral antibiotics. Her blood pressure is 60/45mm Hg and pulse is 120/min. On examination, she appears emaciated and lethargic. Despite numerous attempts, it is impossible to start a peripheral intravenous line, and the child's condition continues to deteriorate. What is the best next step to obtain IV access in this patient?
Intraosseous
Jugular cut down
Femoral vein
Fluids down endotracheal tube
Subclavian central line

A 13-year-old develops fever, malaise, sore throat, and a dry, hacking cough over several days. He does not appear to be particularly sick, but his chest examination is significant for diffuse rales and rhonchi. The chest radio- graph is shown below. Which of the following is the most likely pathogen?
Mycobacterium tuberculosis
Mycoplasma pneumoniae
Streptococcus pneumoniae
Haemophilus influenzae
Staphylococcus aureus
A 6-week-old child is being evaluated for a fever of unknown etiology. As part of the laboratory evaluation, a urine specimen was obtained that grew E coli with a colony count of 2000/µL. These findings would be definite evidence of a urinary tract infection if which of the following is true about the sampled urine?
It is the first morning sample
It has a specific gravity of 1.008
It is from an ileal-loop bag
It is from a suprapubic tap
It is from a bag attached to the perineum of an uncircumcised boy
A 5-day-old male term neonate has been passing maroon-colored stools for the past three days, along with frequent episodes of vomiting. He is being breastfed by his mother, who is an asthmatic. His vital signs are within normal limits. The physical examination is unremarkable. Stool examination is positive for RBCs and eosinophils. What is the most likely cause of this patient's findings?
Milk protein intolerance
Hirschsprung's disease
Necrotizing enterocolitis
Meckel's diverticulum
Viral gastroenteritis
A 4-month-old child is admitted to the hospital for evaluation of failure to thrive and generalized seizures. On physical examination, the child appears wasted and has a protuberant abdomen and marked hepatomegaly. Laboratory evaluation reveals fasting hypoglycemia, lactic acidosis, hyperuricemia, and hyperlipidemia. The boy's parents are first cousins. Of the following, the BEST long-term management of this disorder is
Regular oral administration of cornstarch
Oral dietary supplementation with long-chain fatty acids
Oral dietary supplementation with protein
Regular intravenous administration of glucagon
Regular intravenous administration of 10% dextrose in water
An 11-year-old girl is brought to the office by her mother due to headaches for the last 4 hours. The headaches are bifrontal, and are accompanied by nausea, vomiting, and sensitivity to light and noise. It is her second episode, and both episodes were preceded by dark spots in her visual field. The first episode was 2 weeks ago. She doesn't report any numbness or tingling in her extremities, and no behavioral change or decline in school performance was noted. Her vital signs are stable, and she is afebrile. The physical examination is normal. What is the most appropriate next step in the management of this patient?
Reassurance and acetaminophen
MRI of the brain
CT scan of the head
Electroencephalogram
Lumbar puncture
An anxious 16-year-old girl presents to the emergency department complaining of a sudden onset of feeling that she is unable to breathe. She also complains of tingling around her lips and fingertips. Upon further questioning, you learn that she has had frequent similar episodes in the past. She has no history of asthma, and she has no chest pain or fever. Physical examination reveals a respiratory rate of 30 to 40 breaths/min, oxygen saturation on room air of 99%, no intercostal retractions, and no fever. No wheezing or crackles are evident on chest auscultation; breath sounds are good bilaterally. The balance of findings on the physical examination, including a complete neurologic evaluation, are normal. Of the following, the symptom that BEST distinguishes the correct diagnosis from compensatory hyperventilation is
Chronicity of the complaint
Lack of chest pain
Respiratory rate
Oxygen saturation
Lack of fever
The parents of a child who was diagnosed at birth with Beckwith-Wiedemann syndrome bring in the baby for his 2-month evaluation. They ask about future health problems and his prognosis now that his omphalocele has been repaired. Of the following, the child is MOST at risk for
Acute lymphocytic leukemia
Wilms tumor
Rhabdomyosarcoma
Astrocytoma
Hodgkin disease
A 4-month-old boy presents to the clinic with a 2-day history of a temperature of 100.6°F (38.1°C) and vomiting. The infant was born at 26 weeks' gestation, and his birthweight was 960g. He remained in the hospital for 3 months after birth because of multiple complications, including bilateral grade 4 intraventricular hemorrhages necessitating the placement of a ventriculoperitoneal shunt 6 weeks ago. Physical examination reveals an afebrile infant who has a shunt bubble on the right temporo-occipital region and a gastrostomy button. You explain that his shunt bubble requires aspiration to evaluate the cerebrospinal fluid for infection. Of the following, the organism that is MOST likely to be isolated in the aspirate is
Nontypeable Haemophilus influenzae
Staphylococcus epidermidis
Enterococcus sp
Streptococcus pneumonia
Escherichia coli
A 14-year-old girl was seen in accident and emergency following her third collapse this year and referred to cardiology for review of a low rumbling murmur heard at the left upper sternal edge. Her ECG in accident and emergency was normal. Her blood sugar was 5.3 mmol/L. Urea and electrolytes were normal. The most recent collapse occurred at school while waiting for exam results to be given out. Previously they occurred while watching a parade all afternoon standing in a crowded street, and at a party. On all three occasions she felt dizzy beforehand, was unconscious for less than 10 seconds and fully alert following the episode, but did feel nauseous. Her echocardiogram today is normal. What is the most likely diagnosis?
Wolff–Parkinson–White syndrome
Venous hum murmur and vasovagal syncope
Innocent murmur and epilepsy
Patent foramen ovale and sick sinus syndrome
Neurocardiogenic syndrome
A pediatrician examines a 2-month-old infant who had been born at term. The pediatrician hears a continuous murmur at the upper left sternal border. The peripheral pulses in all extremities are full and show widened pulse pressure. Which of the following is the most likely diagnosis?
Coarctation of the aorta
Patent ductus arteriosus
Persistent truncus arteriosus
Peripheral pulmonic stenosis
Ventricular septal defect
A 12-year-old girl has had a sore throat over 2 days. She now has a fever of 39.5°C and has difficulty opening her mouth, swallowing, or speaking. Her throat can be visualized with difficulty, the right tonsil is significantly more enlarged than the left, and the uvula is displaced to the left side. Which of the following is the most likely diagnosis?
Acute pharyngitis
Peritonsillar abscess
Lateral pharyngeal abscess
Acute uvulitis
Retropharyngeal abscess

You are called to the newborn nursery to evaluate a term infant with bilious emesis. Although the mother had poor prenatal care, she had a normal vaginal delivery with no complications. The infant began having bilious vomiting several hours after birth. The infant has urinated, but has not had a bowel movement. Vital signs are temperature 36.9 0C (98.4 0F), pulse 150/min, and respiratory rate 40/min. On examination, the abdomen is distended and there are decreased bowel sounds. The remainder of the physical examination is unremarkable. An abdominal radiograph is shown below. Which of the following is the most likely diagnosis?
Intestinal atresia
Necrotizing enterocolitis
Hirschsprung disease
Pyloric stenosis
Gastroesophageal reflux
A healthy 1-year-old child comes to your office for a routine checkup and for immunizations. His parents have no complaints or concerns. The next day, the CBC you performed as customary screening for anemia returns with the percentage of eosinophils on the differential to be 30%. Which of the following is the most likely explanation?
Bacterial infections
Tuberculosis
Helminth infestation
Fungal infections
Chronic allergic rhinitis
A 22-year-old woman has just delivered a male infant at 41 weeks of gestation. Her medical history is normal and her pregnancy was uncomplicated. She is an assistant in a veterinary clinic. Examination of the infant reveals jaundice, hepatosplenomegaly, and generalized lymphadenopathy. During the examination, he suddenly begins to have tonic-clonic seizures. The CT scan reveals active inflammatory lesions, hydrocephalus and intracranial calcifications. What is the most likely diagnosis of this patient?
Congenital herpes simplex
Congenital rubella
Congenital syphilis
Congenital hepatitis B
Congenital toxoplasmosis
A 16-year-old girl comes to the physician's office because she has not begun menstruating yet. Both her mother and an older sister started menstruation at age 12. She takes no medication and denies strenuous exercise or excessive dieting. Her height is at the 50fh percentile for age; her weight is at the 60fh percentile. Both her breast and pubic hair development are at Tanner stage 4. Pelvic ultrasonography reveals a normal uterus and ovaries. Which of the following is the most likely diagnosis?
Testicular feminization syndrome
Physiologic pubertal delay
Imperforate hymen
Prolactinoma
Turner syndrome
The mother of a 14-year-old boy arranges to meet with you privately before the boy's annual health supervision visit. She is concerned because he is quiet, has no athletic interests, and has only a few friends. He is content to spend the weekend shopping, cooking, reading, and listening to music. Although he doesn't like school, he is an honor student. The mother also tells you her husband's youngest brother recently disclosed his homosexuality and wants to introduce his male partner to the extended family. Of the following, while counseling the mother, you are MOST likely to include a statement that
Sexual orientation is culturally determined
Self-awareness of sexual orientation is established by age 5 years
She should explain to her son that he is free to choose his sexual orientation
Sexual play with same-sex friends is a clear marker for homosexuality
Compared with heterosexual peers, gay high school students are more likely to abuse substances
A 5-year-old boy is brought to the emergency department by his mother. One week ago, he developed a low grade fever followed by persistent bouts of coughing that last 20-30 minutes each. The coughing spells are severe, unresponsive to antitussive medications, and appear to worsen with eating and drinking cold liquids. On physical examination, there is subconjunctival hemorrhage and extensive subcutaneous emphysema over the anterior chest. What is the most likely organism responsible for this child's illness?
Bordetella pertussis
Pseudomonas
Rickettsia rickettsia
Actinomyces
Haemophilus influenza
A 12-year-old girl with a history of asthma has been admitted to intensive care units two times in the past and has had three emergency department visits during the past 12 months. Her only medication is inhaled albuterol as needed, and she uses it two to three times a day. She has nocturnal symptoms about two times a week. She is free of symptoms now but reports that she gets short of breath easily. Which of the following pharmacologic interventions is most appropriate?
Inhaled corticosteroid
Anticholinergic agent
Nedocromil sodium
Cromolyn sodium
Long-term bronchodilato
A 17-year-old girl presents to the office with a 5-day history of a malodorous vaginal discharge. She is sexually active and uses condoms for sexual intercourse. On examination, a thin, white discharge is seen. A "fishy" odor is produced when KOH is added to the discharge. The vaginal fluid has a pH of 5. Which of the following is the most likely finding on a microscopic examination of the vaginal fluid?
Pseudohyphae
Lactobacilli
Trichomonads
Gram-negative diplococc
Clue cells
Parents bring a 5-day-old infant to your office. The mother is O negative and was Coombs positive at delivery. The term child weighed 3055 g (6 lb, 1 oz) at birth and had measured baseline hemoglobin of 16 g/dL and a total serum bilirubin of 3 mg/dL. He passed a black tarlike stool within the first 24 hours of life. He was discharged at 30 hours of life with a stable axillary temperature of 36.5°C (97.7°F). Today the infant’s weight is 3000 g, his axillary temperature is 35°C (95°F), and he is jaundiced to the chest. Parents report frequent yellow, seedy stool. You redraw labs and find his hemoglobin is now 14 g/dL, and his total serum bilirubin is 13 mg/dL. The change in which of the following parameters is of most concern?
Body weight
Temperature
Bilirubin
Stool
Hemoglobin
A 2-month-old infant is brought to the emergency department with irritability and lethargy. The parents state that he was well until he rolled off the couch on to the floor yesterday. On examination, he is inconsolable and afebrile. The fontanels are full and tense. He has a generalized tonic-clonic seizure. Which of the following is the most important initial diagnostic study to order?
Serum ammonia level
Serum acetaminophen level
Analysis of cerebrospinal fluid (CSF)
Serum calcium, phosphorus, and magnesium levels
Cranial computed tomography (CT) scan
A 16-year-old female presents to the emergency room with severe right- sided abdominal pain. Her last menstrual period was 2 weeks ago and felt to be normal. She displays painful difficulty in positioning herself on the examination table. Her temperature is 38.5 C (101.3 F), blood pressure is 128/75 mm Hg, pulse is 80/min, and respirations are 22/min. Examination of the throat reveals mild pharyngitis. Her abdomen is diffusely tender, especially the lower abdomen. Rectal examination reveals tenderness anteriorly on the right side. Stool guaiac is negative. A pelvic examination is performed, and there is evidence of cervical tenderness and questionable fullness in the right adnexal area. Which of the following is the most likely diagnosis?
Pyelonephritis
Ovarian cyst
Endometriosis
Constipation
Pelvic inflammatory disease
A 3-day-old newborn is ready to be discharged from the neonatal nursery, when his mother reports that a rash has appeared on his abdomen and chest. He otherwise appears healthy. He has no fever and no risk factors for infection. Examination reveals a nontoxic neonate with erythematous papules and vesicles surrounded by patches of erythema. Microscopic evaluation of the pustules reveals numerous eosinophils. What is the most likely diagnosis?
Staphylococcal scalded skin syndrome
Sebaceous hyperplasia
Erythema toxicum
Milia
Neonatal varicella
A 4-year-old boy falls from the jungle gym at preschool. He sustains minor abrasions and contusions, and is taken care of by the school nurse. His parents take him that same afternoon to his regular pediatrician and demand "a thorough check-up" for possible internal injuries. The pediatrician complies, and a complete physical examination is normal. His hemoglobin is 14 g/dL, and a urinalysis shows the presence of microhematuria. Which of the following is the most appropriate next step in management?
Retrograde ureterogram and cystogram
Urologic workup, starting with a sonogram
CT scan of the abdomen and pelvis
Reassure the parents that microhematuria from minor trauma will resolve spontaneously
Serial hemoglobin and hematocrit determinations
A 3-year-old child is rushed to the emergency department after the mother found her with an open and empty bottle of acetaminophen. The mother has no idea how many tablets were in the bottle. She estimates that no more than 1 hour has passed since the child ingested the tablets. The child began to vomit during the trip to the emergency department, and has vomited three times more since her arrival. The child is awake and alert but clearly unhappy, crying even in her mother's arms. She appears pale and diaphoretic. Her heart rate is 110 beats/min, respiratory rate is 26 breaths/min, temperature is 98.6°F (37°C), and blood pressure is 90/60 mm Hg. Of the following, the MOST appropriate statement about acetaminophen toxicity is that:
The administration of activated charcoal is contraindicated in acetaminophen toxicity
An antidote is available, but its use can be deferred until further information is gathere
The contents of one bottle of acetaminophen are not sufficient to cause life-threatening toxicity in a child
Multiple episodes of vomiting indicate that irreversible liver damage already has occurred
Given the short duration since the ingestion, it will be helpful to administer syrup of ipecac
A 15-month-old boy presents to the emergency department following the acute onset of nausea, vomiting, and abdominal pain. He appears agitated. His heart rate is 160 beats/min, but other vital signs are normal. His mother, who has asthma, reports finding her theophylline bottle lying empty on the floor in her bedroom. His capillary blood gas measurement is normal, and his blood glucose concentration is 190 mg/dL (10.5 mmol/L). Of the following, the MOST appropriate management of this patient is
Administration of activated charcoal
Whole-bowel irrigation
Administration of beta-adrenergic receptor antagonists
Gastric lavage
Administration of ipecac
A 5-year-old African-American boy is brought to the office by his mother due to a painful right knee, fever and chills over the last 2 days. The child was diagnosed with pharyngitis 2 weeks ago, and was treated with a 10-day course of penicillin G. His temperature is 38.8 C (102F) and pulse rate is 102/min. On examination, his right knee joint is swollen and erythematous, with a decreased range of motion. The laboratory findings are significant for leukocytosis and an elevated ESR. X-rays of both the right hip and knee joints are normal. What is the most appropriate treatment for the patient's condition?
Bed rest with the right knee joint in a position of comfort
Right knee arthrocentesis & intravenous nafcillin
Bed rest & a ten-day course of penicillin G
Repeat a ten-day course of penicillin G
Bed rest & aspirin
A neonate is noted to have aniridia of the right eye on physical examination. He was born by spontaneous vaginal delivery after an uncomplicated full-term pregnancy. The remainder of the physical examination is normal. Which of the following is the most appropriate next step before the infant is released from the hospital?
TV antibiotics
A neurology consult
An echocardiogram
An abdominal ultrasound
A rapid plasmin reagin (RPR) test
A 10-day-old infant is brought to the office by her mother for the evaluation of purulent discharge from both eyes. The discharge appeared three days ago, after which the child developed a cough. On examination, the infant's eyes appear normal, except for the presence of purulent discharge. Auscultation reveals diffuse rales without wheezing. Chest radiograph shows a hyperinflated thorax. What is the most likely diagnosis?
Gonococcal conjunctivitis
Congenital chlamydial infection
Chemical conjunctivitis
Congenital rubella infection
Adenovirus infection
A full-term newborn develops cyanosis a few hours after birth. Oxygen administration does not improve color or oxygen saturations. Which of the following is the most likely diagnosis?
Pulmonary stenosis
Aortic stenosis
Ventricular septal defect
Patent ductus arteriosus
Atrial septal defect
A 16-year-old girl is being evaluated for primary amenorrhea. Her birth history is significant for low birth weight and bilateral swelling of the hands and feet. Her blood pressure is 170/96 mmHg. She has a short stature and webbed neck. Her karyotype examination results show 22 pairs of autosomes, one X, and one Y chromosome. Which of the following statements is true regarding this patient's condition?
The girl should undergo bilateral abdominal gonadectomy
The primary amenorrhea in this girl is most likely caused by functional uterine abnormalities
This child will benefit from steroid hormone replacement therapy
The webbing of the neck is caused by defects in arteriovenous communications
The inheritance for this condition is Mendelian dominant
A 6-year-old boy presents in clinic for a routine visit. Examination reveals coarse, dark pubic hair, an enlarged penis and testes, and acne of the face and upper back. His mother notes that he has a body odor similar to that of her teenage son after playing sports. The child is in file 99th percentile of height for his age group. Which of the following is the most likely diagnosis?
Male pseudohermaphroditism
Hypothalamic tumor
XYY syndrome
Klinefelter syndrome
Congenital adrenal hyperplasia
A 4-year-old boy was diagnosed with nephrotic syndrome 6 months ago and has required a long course of oral corticosteroids to maintain remission of the condition. He has developed truncal obesity and you are concerned he may be developing Cushing’s syndrome. Which of the following is not a complication of Cushing’s syndrome?
Hypertension
Osteoporosis
Short stature
Hypoglycaemia
Gastric irritation
A mother brings her daughter into the clinic for a routine health-care visit. On examination, you note that she walks alone, knows two words, throws objects, and comes when called. What is the most likely age of this infant?
6 months
15 months
9 months
18 months
12 months
A 2-month-old infant is evaluated by a pediatric cardiologist. The infant was noted at birth to have an upper left sternal border ejection murmur. The infant at that time was not cyanotic, but slowly developed cyanosis over the next two months. At the time of the pediatric cardiologist's examination, an ECG showed right axis deviation and right ventricular hypertrophy. A chest x-ray film showed a small heart with a concave main pulmonary artery segment and diminished pulmonary blood flow. Which of the following is the most likely diagnosis?
Hypoplastic left ventricle
Tetralogy of Fallot
Isolated atrial septal defect
Transposition of the great arteries
Complete atrioventricular canal defect
A 15-year-old girl comes to accident and emergency complaining of sudden right arm weakness and double vision. Last week she was incontinent of urine twice. She is normally fit and well. On examination she has a left-sided 6th nerve palsy and four out of five power in her right arm. The examination is otherwise unremarkable. An MRI head shows multiple hyperintense, inflammatory, white matter lesions. What is the most likely diagnosis?
Multiple sclerosis
Tuberous sclerosis
Neurofibromatosis
Tuberculous meningitis
Brain metastasis
A 10-year-old presents with 2 months history of heavy menstrual-like bleeding. Menarche occurred 6 months ago and this first menses consisted of spotting for 3-4 days without cramps. Subsequent periods were light in flow but lasted 6 to 8 days. Which of the following is the most likely cause of her bleeding?
Pregnancy
Dysfunctional uterine bleeding
Thyroid disease
Ovarian tumor
Von Willebrand disease
A mother with known placenta praevia with heavy vaginal bleeding was rushed into the labour ward and delivered by emergency caesarean section at 35 weeks’ gestation. Pre-delivery the fetus was bradycardic and after birth APGARs were three at 1 minute, five at 5 minutes and nine at 10 minutes. Thirty-six hours later on the special care baby unit the baby is irritable and requiring nasogastric tube feeds as he is not sucking well. The tone in his upper limbs is reduced and an EEG showed seizure activity which has been controlled by intravenous phenobarbitone. His cranial ultrasound is normal. His blood sugar monitoring is between 3.5 and 5 mmol/L, C-reactive protein (CRP) was less than 5 mg/L and is 7 mg/L today. He is apyrexial. What is the most likely diagnosis?
Mild hypoxic ischaemic encephalopathy (HIE)
Hypoglycaemia
Intraventricular haemorrhage
Group B streptococcal meningitis
Moderate HIE
An infant born at term to a 22-year-old woman has a weak cry and is cyanotic at birth. His fingertips and oral mucosa appear blue. His blood pressure is 80/40 mmHg and his heart rate is 140/min. Chest x-ray shows clear lung fields bilaterally. PaO2 measured by arterial cannulation is 38 mmHg, and improves only minimally on 100% inspired oxygen. Which of the following is the best next step in managing this patient?
Loop diuretics
Prostaglandin E1 infusion
Low dose beta-blocker
Single dose of indomethacin
Packed red blood cell transfusion
A 2-week postmature neonate exhibits severe respiratory distress immediately after birth. Previously, greentinged meconium was noted in the amniotic fluid. Which of the following is the most appropriate next step in management?
Oxygen supplementation by face mask
Suctioning of the mouth and nasopharynx
Intubation with mechanical ventilation
Chest x-ray
Emergency tracheostomy
An 8-year-old boy is brought to his physician by his mother, who is worried by the child's frequent episodes of daydreaming, which have apparently resulted in a decline in school performance. The child's psychomotor development appears normal. EEG recording reveals bilateral and symmetric 3 Hz spike-and-wave discharges, which begin and end abruptly on a normal background. Which of the following is the most likely diagnosis?
Pseudoseizures
Absence seizures (petit mal)
Tonic-clonk seizures (grand mal)
Complex partial seizures
Simple partial seizures
You receive a telephone call from the mother of a 4-year-old child with sickle-cell anemia. She tells you that the child is breathing fast, coughing, and has a temperature of 40°C (104°F). Which of the following is the most conservative, prudent course of action?
Refer the child to the laboratory for an immediate hematocrit, white blood cell count, and differential.
Prescribe aspirin and ask her to call back if the fever does not respond.
Admit the child to the hospital.
Make an office appointment for the next available opening.
Make an office appointment for the next day.
A 6-year-old girl presents to hospital with a large right-sided abdominal mass. It does not cross the midline. On further questioning she has had macroscopic haematuria and weight loss of 4kg over the last 4 months. She has reduced appetite and lethargy. Her blood pressure is 125/73 mmHg, heart rate 120 bpm. Which of the following is not a complication of this malignancy?
Metastatic spread
Renal impairment
Urinary catecholamines
Malnutrition
Hypertension
A 4-week-old boy has been vomiting all of his feedings for the last 2 days. His mother reports decreased urine output but no fever. On physical examination, he is alert, appears hungry, and is moderately dehydrated. Abdominal examination reveals a small mass in the epigastrium. When he is offered a bottle, he takes it vigorously and then vomits forcefully. You order laboratory tests. Of the following, the MOST likely abnormality to expect is
Hyperkalemia
Metabolic acidosis
Hypernatremia
Hyperchloremia
Metabolic alkalosis
Over the past week, you and your colleagues have seen a number of previously healthy children younger than 2 years of age who present with fever, coryza, cough, vomiting, and diarrhea. Several of the children have required hospitalization for respiratory distress and pneumonia. You suspect that influenza virus infection is the cause of these illnesses. Of the following, the MOST rapid test to confirm the diagnosis in these patients is
Immunoglobulin M (IgM) titers on acute sera
Polymerase chain reaction
Enzyme immunoassay antigen detection
IgM titers on acute and convalescent sera
Viral culture
The parents of a 14-year-old boy are concerned about his short stature and lack of sexual development. By history, you learn that his birth weight and length were 3 kg and 50 cm, respectively, and that he had a normal growth pattern, although he was always shorter than children his age. The physical examination is normal and his growth curve is shown on the next page. His upper-to-lower segment ratio is 0.98. A small amount of fine axillary and pubic hair is present. There is no scrotal pigmentation; his testes measure 4.0 cm3 and his penis is 6 cm in length. In this situation, which of the following is the most appropriate course of action?
Reassure the parents that the boy is normal
Biopsy his testes
Measure pituitary gonadotropin
Measure serum testosterone levels
Obtain a computed tomographic (CT) scan of the pituitary area
A 5-day-old baby is brought to see the GP because she has had a rash for the past 3 days which started on her chest, is spreading to her face and getting worse. On examination she handles well and is alert. There is an erythematous rash on her face, torso and right arm with little pustules. What is the most likely diagnosis?
Infected eczema
Neonatal acne
Erythema toxicum
Neonatal sepsis
Molluscum contagiosum
A 3-week-old female is brought into the emergency department with a fever and irritability. She was born after a normal pregnancy and delivery. Her mother had routine prenatal care and has no history of sexually transmitted infections. The infant's mother is 14 years old and the father is 17 years old. They are not married, and the father is not involved in the care of the infant. The infant lives with her mother and maternal grandparents at the maternal grandparents' home. You are concerned about meningitis and decide to do a lumbar puncture. The mother and maternal grandparents are present in the emergency department. Informed consent should be obtained from which of the following individuals?
Mother and father must both provide consent
Maternal grandparents since the mother is a minor
Mother and grandparents since the mother is a minor
Informed consent is not necessary because the mother is a minor
Mother
A 2-year-old child is brought to the office by his parents for the evaluation of failure to thrive and chronic diarrhea. His diarrhea is "almost continuous", and he also has recurrent episodes of fever. He was initially quite well and was on the 60th percentile for weight; however, for the past seven months, he didn't seem to grow and failed to gain weight. Over the past three months, he fell to the 3rd percentile for weight. His parents deny any use of drugs, but they drink occasionally. His mother mentions that her former boyfriend was a heroin addict. Physical examination reveals oral thrush, generalized lymphadenopathy and eczema. What is the most likely diagnosis in this patient?
Malabsorptive disease
HIV infection
Congenital Toxoplasmosis
Non-Hodgkin lymphoma infiltrating small intestine
Miliary tuberculosis
You receive a call from a teenage patient, who tells you that she is having palpitations and feels somewhat lightheaded. You refer her to your local emergency department, where no symptoms are discerned and physical examination findings are normal. The emergency department sends a copy of the patient's electrocardiogram by facsimile to your office for you to review. Of the following, the BEST interpretation of the girl's electrocardiogram is
Supraventricular tachycardia
Premature atrial contractions
Premature ventricular contractions
Wolff-Parkinson-White syndrome
Ventricular tachycardia

You are seeing a 2-year-old boy for the first time. His father denies any past medical or surgical history, but does note that the child’s day care recently sent a note home asking about several episodes, usually after the child does not get what he wants, when he “breathes funny” and sits in a corner with his knees under his chin for a few minutes. The day-care staffers think this “self-imposed time-out” is a good thing, but they worry about the breathing. One teacher even though he once looked blue, but decided that it was probably because of the finger paints he had been using. On examination, you identify a right ventricular impulse, a systolic thrill along the left sternal border, and a harsh systolic murmur (loudest at the left sternal border but radiating through the lung fields). His chest radio- graph and ECG are shown. Which of the following congenital cardiac lesions would you expect to find in this child?
Transposition of the great vessels with a patent foramen ovale
Right ventricular outflow obstruction
Hypoplastic left heart
Patent ductus arteriosus
Atrial septal defect (ASD)
A 16-year-old girl is being seen in your clinic because of headaches for the past month that sometimes awaken her at night. At her last visit 2 years ago, she was well, 5 ft 2 in tall, and weighed 105 lb, with Sexual Maturity Rating (SMR) 4 breast development and SMR 4 pubic hair, but she had not reached menarche. On examination at this visit, she is 5 ft 2 in tall, weighs 110 lb, and still has not begun menstruating. On evaluation, you note bitemporal visual field deficits, perhaps worse on the left. In addition to magnetic resonance imaging and an ophthalmologic evaluation, the laboratory test that is MOST likely to be most diagnostically revealing is
Insulin-like growth factor-1
Luteinizing hormone
Prolactin
Thyroid-stimulating hormone
Adrenocorticotropic hormone
A 2-year-old boy has been vomiting intermittently for 3 weeks and has been irritable, listless, and anorectic. His use of language has regressed to speaking single words. In your evaluation of this patient, which of the following is the most reasonable diagnosis to consider?
Expanding epidural hematoma
Bacterial meningitis
Tuberculous meningitis
Food allergy
Herpes simplex virus (HSV) encephalitis
A 7-year-old girl was found in a routine health supervision visit to have bilateral breast tissue development. She also had long, pigmented hair over the labia majora. Her height and weight are both at the 80th percentile for her age. Which of the following is the most appropriate management?
Thyroid stimulating hormone (TSH) level
Radiography of the head and wrist
Reassurance to the parents that it is normal
CT of the head and abdomen
Pelvic ultrasonography
A 15-year-old girl is rushed to the emergency department after slipping off a diving board and striking her head on cement. On physical examination, her mental status evaluation results are completely normal. She can abduct her upper extremities at the shoulder, but cannot flex or extend her arms and minimally moves her fingers. She cannot move her limp lower extremities. You order emergent magnetic resonance imaging of the brain and spine. Of the following, the MOST important therapy to implement before the patient is sent for imaging is
Methylprednisolone 30 mg/kg intravenously
Mannitol 1 g/kg intravenously
Fosphenytoin 18 phenytoin equivalents/kg intravenously
Low-molecular weight heparin 1 mg/kg subcutaneously
Dexamethasone 1 mg/kg orally
A 2-year-old girl presents with fever of 39.3 C and irritability. She has had an upper respiratory tract infection for 4 days. On examination, the right ear is bulging and has poor movement on insufflation. Which of the following organisms is most likely responsible for these findings?
S. aureus
S. pneumoniae
M. pneumoniae
E. coli
Group A Streptococcus
A 2-year-old boy is admitted to the paediatric ward with a swollen, painful left knee. He has been afebrile and has a history of minor trauma to his knee earlier today. His mother is a haemophilia carrier and his father is not affected. You are keen to rule out haemophilia in this child. Which two clotting factors should you test for?
Factor V and VI
Factor X and XI
Factor VII and IX
Factor VII and VIII
Factor VIII and IX
A 2-year-old boy has had a purulent drainage from the right nostril for a week. He is afebrile and has had no associated symptoms, such as cough. Which of the following is the most likely diagnosis?
Nasal polyps
An upper respiratory infection
Sinusitis
A foreign body in the right nostril
Allergic rhinitis
Otitis media occurring during the first 8 weeks of life deserves special consideration, because the bacteria responsible for infections during this time may be different from those that affect older infants and children. Which of the following organisms is the most likely to cause otitis media in these infants?
Neisseria gonorrhoeae
Chlamydia trachomatis
Toxoplasma gondii
Treponema pallidum
E. coli
A new born infant is in respiratory distress and requires several attempts at resuscitation in the delivery room because of difficulty breathing and frequent cyanosis. The neonatologist notes that during crying, her breathing improves and breath and heart sounds are normal. Direct laryngoscopy is unremarkable as well. Deep inspirations by the neonate are ineffective. Which of the following is the most effective intervention?
Obtaining an electrocardiogram
Administering atropine
Inserting an oropharyngeal tube
Obtaining a chest x-ray film
Obtaining an arterial blood gas
A 2-year-old boy is brought to the emergency department (ED) in acute respiratory distress. He is afebrile, and has a heart rate of 100/min, respiratory rate of 80/min, and Sa02 of 84% on room air. He is sitting upright, and has significant nasal flaring and intercostal retractions. He is given supplemental oxygen in the ED. Chest x-ray reveal hyperinflation of the right lung, mediastinal shift to the left, and a severely hypoinflated left lung Which of the following is the most appropriate next step in management?
Direct laryngoscopy and rigid bronchoscopy
Direct laryngoscopy and flexible bronchoscopy
CT scan of the chest
Bronchodilator therapy
Segmental lung resection
A 6-month-old infant presents to the emergency department with the new onset of weak cry, decreased activity, and poor feeding. The mother also states that the infant has been constipated for the past 2 days. On physical examination, the infant has a very weak cry, poor muscle tone, and absent deep tendon reflexes. Which of the following is the most likely diagnosis?
Vaccine-associated poliomyelitis
Myasthenia gravis
Congenital hypothyroidism
Guillain-Barré syndrome
Infant botulism
A 4 year old is brought to accident and emergency acutely unwell and refusing to walk for the past 2 days. Her parents are not aware of any recent injuries. On examination, she is pyrexial (T = 39.2°C), capillary refill 3 seconds centrally, heart rate 150 beats per minute, respiratory rate 40 breaths per minute. Her right thigh is swollen and slightly erythematous but too tender to examine fully. An x-ray of the hip and femur shows soft tissue swelling surrounding the proximal femur but the bones look normal. An urgent MRI shows a periosteal reaction in the proximal femur with extensive inflammation in the surrounding soft tissues. What is the most likely diagnosis?
Non-accidental injury
Osteomyelitis
Juvenile idiopathic arthritis
Cellulitis
Reactive arthritis
During the health supervision visit for a 1-month-old infant, you note mild jaundice, but no fever and clear lungs. Cardiac examination demonstrates a 2/6 systolic murmur at the left sternal border. Abdominal examination demonstrates a firm liver 3 cm below the costal margin and extending past the midline. The alanine aminotransferase is 140 U/L, aspartate aminotransferase is 130 U/L, total bilirubin is 5.5 mg/dL (94.1 mcmol/L), and direct bilirubin is 3.0 mg/dL (51.3 mcmol/L). Of the following, the finding that MOST strongly suggests the need for referral to a surgeon for intraoperative cholangiography is
Dimethyl iminodiacetic acid scan demonstrating no tracer in the bowel
Brain computed tomography scan demonstrating cerebral calcifications
Echocardiography demonstrating pulmonary artery stenosis
Liver biopsy demonstrating periodic acid-Schiff stain-positive globules in the hepatocytes
Abdominal ultrasonography demonstrating a prominent gallbladder
You are seeing a 6-week-old infant who was born with trisomy 21 and a large atrioventricular septal defect. Over the previous week, she has tired with feeding and has not gained weight. Her respiratory rate is 60 breaths/min and heart rate is 150 beats/min. Auscultation reveals mild retractions and a 2/6 systolic murmur with a gallop rhythm. The liver is palpable at 2 cm below the costal margin, and the perfusion is good. You decide to increase the caloric content of the formula to 24 kcal/oz, and you contact her pediatric cardiologist to discuss referral for surgical repair. Of the following, the BEST therapeutic option while awaiting surgical repair is
Hydralazine
Captopril
Furosemide
Propranolol
Verapamil
A 4-year-old, apparently healthy child is examined by a pediatrician. The pediatrician hears a loud systolic ejection murmur with a prominent systolic ejection click. He also hears a soft, early diastolic murmur. Both murmurs are heard best at the upper right sternal border. ECG shows left ventricular hypertrophy. Which of the following is the most likely diagnosis?
Atrial septal defect
Transposition of great arteries
Aortic valve stenosis
Tetralogy of Fallot
Ventricular septal defect
A 1-year-old child is brought in for a regular "well baby" check-up. The child appears to have strabismus. The reflection of a bright light from the ceiling of the examination room comes from a different place in each eye. The family explains that the child has always looked that way, and there has been no recent change in the appearance of his eyes. Which of the following is the most effective management?
Surgical correction as soon as it is practical to do it
Surgical correction whenever he is old enough to decide whether he wants it for cosmetic reasons
Each eye patched for a month at a time, alternating sides
Corrective lenses
No treatment unless the condition has not resolved spontaneously by age 7
A 6-year-old boy with a history of anaphylaxis to peanuts is brought in by ambulance unconscious. He was attending a children’s birthday party. His mother says there was a bowl full of candy and he may have eaten a Snickers bar but she is not sure and she did not have his EpiPen with her. His face and lips are swollen and erythematous, he is still breathing but weakly and there is wheeze. His pulse is tachycardic and thready. Which type of shock is this?
Cardiac
Distributive
Obstructive
Septic
Hypovolaemic
An 8-month-old previously preterm infant with bronchopulmonary dysplasia presents to the emergency department with lethargy. His regular medications include furosemide and spironolactone. His temperature is 37.4 C (99.3 F), blood pressure is 68/32 mm Hg, pulse is 110/min, and respirations are 10/min. He has poor skin turgor and dry mucous membranes. Laboratory chemistry evaluation reveals: sodium, 131 mEq/L; potassium, 3.0 mEq/L; chloride, 84 mEq/L; bicarbonate, 38 mEq/L; blood urea nitrogen, 36 mg/dL; and creatinine, 0.4 mg/dL. An arterial blood gas shows pH, 7.52; PaCO2: 49 mm Hg; and PaO2: 92 mm Hg. Which of the following is the most likely explanation for these findings?
Primary hyperaldosteronism
Volume depletion
Bartter syndrome
Pseudohyperaldosteronism
Primary respiratory acidosis with metabolic compensation
A 12-month-old male infant presents for an ear re-evaluation 1 month after being treated for his fourth episode of otitis media. His parents describe a normal birth history and normal development. The child is breastfed and does not attend child care. His immunizations are up to date through 6 months of age, including three doses of the conjugated pneumococcal vaccine. There is no history of sinusitis, pneumonia, sepsis, meningitis, or urinary tract infections. After the boy's last otitis media infection, your colleague measured the child's serum immunoglobulin (Ig) concentrations, and results included a low IgG of 150 mg/dL (1.5 g/L), a normal IgM of 80 mg/dL (0.8 g/L), and a normal IgA of 40 mg/dL (0.4 g/L). Of the following, the next BEST laboratory test to evaluate this infant's antibody function is
Delayed-type hypersensitivity testing
Nitroblue tetrazolium test
Serum protein electrophoresis
B- and T-cell flow cytometry
Isohemagglutinins
A one-month-old infant is born with craniofacial anomalies. Further evaluation reveals a cognitive impairment, a 22q 11 microdeletion in his chromosomes, and a heart condition with a right-to-left shunt. The infant subsequently undergoes heart surgery. The surgeon notes that the patient's thymus is absent. The anesthesiologist observes prolonged QT intervals in the patient's ECG. What is the most important parameter that should be monitored throughout this surgery?
Potassium levels
Coagulation parameters
Lymphocyte count
Calcium levels
Platelet count
A 9-year-old African-American boy is brought to ER with high fever, poor appetite, and irritability. His heart rate is 140/min and his blood pressure is 80/60 mmHg. He has been hospitalized several times before for poorly localized abdominal pain. He also has a history of hematuria. The boy has not received several routine vaccinations because his mother is afraid that they will cause autism. His hematocrit is 22% and the reticulocyte count is 12%. The patient dies several hours after the admission. This patient's death may have been prevented by which one?
Vaccination with a conjugate capsular polysaccharide
Periodic blood transfusions
Folic acid supplementation
Vaccination with a bacterial toxoid
Vaccination with a live attenuated virus
The parents of a 7-day-old infant bring her to your office for a swollen eye. Her temperature has been normal, but for the last 2 days she has had progressive erythema and swelling over the medial aspect of the right lower lid near the punctum. Her sclera and conjunctiva are clear. Gentle pressure extrudes a whitish material from the punctum. Which of the following ophthalmic conditions is the correct diagnosis?
Hyphema
Congenital Sjögren syndrome
Chalazion
Preseptal cellulitis
Dacryocystitis
A 1-month-old baby boy has bloody diarrhea. No infectious agent is identified, but the baby is found to be profoundly thrombocytopenic. The baby is also noted to have a skin rash, and a dermatologist diagnoses eczema. By three months of age, the baby begins to develop recurrent respiratory infections. If this child survives until adolescence, he is at particularly high risk of developing which of the following?
Wilms tumor
Rheumatoid arthritis
Lymphoma
Congestive heart failure
Crohn disease
The parents of an 8-year-old girl who has asthma would like to know more about possible triggers. The girl has had mild persistent asthma since age 5 years and frequently has increased symptoms in the fall that coincide with starting school. During the fall, she experiences increased rhinorrhea, sneezing, and ocular pruritus. These nasal and ocular symptoms have occurred each fall for the past 3 years but generally do not occur at other times of the year. Of the following, the MOST likely trigger for the patient's asthma exacerbations is
Exercise
Gastroesophageal reflux
Psychogenic cough
Allergic rhinitis
Sinusitis
A 10-month-old baby boy, recently adopted from Guyana, has a 5-hour history of crying, with intermittent drawing up of his knees to his chest. On the way to the emergency room he passes a loose, bloody stool. He has had no vomiting and has refused his bottle since the crying began. Physical examination is noteworthy for an irritable infant whose abdomen is very difficult to examine because of constant crying. His temperature is 38.8C (101.8F). The rectal ampulla is empty, but there is some gross blood on the examining finger. Which of the following studies would be most helpful in the immediate management of this patient?
Air contrast enema
Stool culture
Examination of the blood smear
Coagulation studies
Examination of the stool for ova and parasites
A 2-year-old who has a history of repaired biliary atresia presents to your office with fatigue and intermittent dark stools. On physical examination, he is afebrile and pale but active. His heart rate is 110 beats/min, liver and spleen are both enlarged, and abdomen is distended, with prominent abdominal veins. The hematocrit is 22% (0.22). Of the following, the MOST appropriate next step is to
Begin oral iron supplementation
Arrange for outpatient endoscopy
Obtain abdominal ultrasonography
Refer the boy for therapeutic paracentesis
Arrange for hospital-based care
A previously healthy 15-month-old girl is brought to the emergency department after she had several episodes in which she lost consciousness after crying. Her parents state that the episodes always occur when the child gets frustrated or upset. She has no cyanosis or incontinence. The episodes last about 45 seconds each. After the episode, she is alert and appropriate. Physical examination is unremarkable. What is the next best step in the management of this patient?
Reassure the parents
Obtain an electrocardiogram
Magnetic resonance imaging of the brain
Obtain an electroencephalogram
Computed tomography of the head
A 14-month-old girl is brought to the emergency department with a 12-hour history of fever and rash. Her mother became frightened when it was difficult to arouse the girl after her nap. Findings on physical examination include a temperature of 104°F (40°C), a heart rate of 164 beats/min, a respiratory rate of 42 breaths/min, and a blood pressure of 75/45 mm Hg. There are petechiae and purpura (Item Q156A) on the chest, arms, and legs. As you are establishing intravenous access and drawing blood for initial laboratory evaluations, you request an immediate dose of antibiotics. Of the following, the MOST appropriate therapy is
Vancomycin plus ceftriaxone
Ceftriaxone
Vancomycin plus gentamicin
Vancomycin
Penicillin
A 9-year-old boy is brought to the office by his parents due to headaches, vomiting and visual disturbances. One week ago, he began to experience headaches that were most prominent in the morning. He also became lethargic, and had a decreased appetite and decline in school performance. The pertinent physical findings include an unbalanced gait, trunk dystaxia, horizontal nystagmus, and papilledema. If this child had a medulloblastoma, which structure would most likely be affected?
Spinocerebellar tracts
Cerebellar vermis
Cerebellar hemispheres
Cerebellar peduncles
Frontal lobe
A 12-year-old girl presents to your office for the first time with a swollen, painful, erythematous right knee joint. She tells you that her left knee felt and looked similar yesterday, but now feels normal. She also is easily fatigued and has had fever. On physical examination, she has a temperature of 101.7°F (38.7°C), a heart rate of 125 beats/min, a respiratory rate of 24 breaths/min, and a blood pressure of 120/78 mm Hg. Her lungs are clear. On auscultation, you note a 3/6 holosystolic murmur (Item Q87A) at the cardiac apex with radiation to the axilla. Of the following, the BEST plan for management of this patient's joint swelling includes
Heat, elevation, and splinting of the right knee
Antibiotic therapy with doxycycline
Anti-inflammatory therapy with aspirin
Aspiration of the right knee joint
Immunotherapy with azathioprine
You find a discrete, whitish polyp that extends through the tympanic membrane in a child with a history of recurrent otitis media. This most likely represents which of the following?
Tympanosclerosis
Acute otitis media with perforation and drainage
A cholesteatoma
Dislocation of the malleus from its insertion in the tympanic membrane
Excessive cerumen production
A neonate is markedly edematous and dies 1 hour after birth. A diagnosis of hydrops fetalis is made after the hematocrit on cord blood is demonstrated to be 5%. The erythrocytes in a smear from the cord blood are markedly hypochromatic. The mother is Rh positive and is known to have alpha-thalassemia trait. The thalassemia status of the father is unknown. Alpha-thalassemia is the suspected cause of the infant's hydrops. Which of the following hemoglobins would most likely be markedly elevated in this infant's blood if this diagnosis were correct?
HbH
HbBarts
HbS
HbC
HbGlower2
A mother brings her 4-week-old baby to see you for the third time. He was born at term by normal vaginal delivery with no complications. You started him on antireflux medicine last week but it has not helped. He is now vomiting his whole feeds and is becoming lethargic and passing less urine and stool. His mother says he is hungry even after he vomits. The practice nurse has weighed him and he has lost 200 g since last week. His mother was breastfeeding him while waiting to be seen and as you go to examine him, the baby has a large milky vomit, which cascades over the clinic floor. What is the most likely diagnosis?
Necrotizing enterocolitis (NEC)
Volvulus
Gastroenteritis
Pyloric stenosis
Intussusception

A very upset mother brings her 8-month-old child to the emergency room because he will not move his leg. She reports that when she was carrying him to the car about half an hour ago, she slipped on some ice and fell on top of him. The mother, an 18-year-old African American woman, has been exclusively breast-feeding her child. She has only recently started him on cereals, and has not supplemented his diet with vitamins. A radiograph of the child’s leg is shown below. Which of the following laboratory findings would be expected?
Hypophosphaturia
Reduced serum alkaline phosphatase
Hypocalcemia
Hyperphosphatemia
Hypocalciuria
A female neonate is undergoing an examination after birth. She was born to a 33-year-old primigravid mother at term via a normal spontaneous vaginal delivery. The pregnancy was uncomplicated, except for a positive maternal group B Streptococcus culture at 36 weeks' gestation, for which the mother received penicillin during labor. The infant's APGAR scores are 8 at 1 minute and 9 at 5 minutes. The mother notices that the infant has prominent labia and a dull pink vaginal epithelium. Which of the following is the most likely cause of the appearance of the infant's genitalia?
Exposure to penicillin
Infection with group B Streptococcus
Sexual abuse
Exposure to maternal estrogen
Infection with Chlamydia

A 7-year-old boy was brought to the emergency department after falling onto his outstretched arm. He complains of pain in his left arm and refuses to move his arm at the elbow. On examination, the left arm is swollen, slightly pale, and edematous. His radial pulse is intact. The patient's radiograph is shown below. While the patient is waiting for the orthopedic resident on call to examine him, he continues to complain of increasing pain despite multiple doses of pain medication. Which of the following should you be most concerned about in this patient?
Transient neuropraxia
Compartment syndrome
Narcotic abuse
Displacement of the fracture
Brachial artery injury
A previously heathy 3-year-old boy is brought to the emergency department (ED) due to stridor of sudden onset. Last night, he suddenly developed a high fever followed by breathing difficulty. His temperature is 40C (104F), pulse is 130/min, and respirations are 40/min. In the ED, the child is toxic-appearing, sitting up, leaning forward and drooling. His lungs are clear, and oxygen saturation is 85% in room air. What is the most appropriate next step in management?
Admit the patient and start him on broad spectrum antibiotics
Admit the patient and start him on nebulized racemic epinephrine
Start the patient on oral dexamethasone
Start the patient on intravenous methylprednisolone
Endotracheal intubation with a set-up for tracheostomy
A 12-year-old girl complains of intermittent palpitations. She had previously been in excellent health and has met all development milestones. There is no family history of heart disease. She is on no medications and takes no drugs. She states that the palpitations begin and end suddenly and usually last a couple of hours. She is otherwise asymptomatic between episodes. The physical examination is normal. An ECG reveals a shortened PR interval and a slow upstroke of the QRS wave in lead III. Which of the following is the most likely diagnosis?
Sinus tachycardia
Lown-Ganong-Levine syndrome
Wolff-Parkinson-White syndrome
Anxiety attack
Nodal reentrant tachycardia
A 4-day old pre term male neonate is being managed in the neonatal intensive care unit. He was born in the 34th week of gestation via lower segment caesarian section. On the first day of life, he developed tachypnea, grunting and nasal flaring. Chest x-rays showed a ground glass appearance of both lungs. He underwent endotracheal intubation and therapy with intravenous fluids, positive pressure ventilation, and intravenous antibiotics. He consequently showed remarkable improvement; however, he is currently beginning to have increased gastric residues. What is the most likely cause for this child's increased gastric residues?
Necrotizing enterocolitis
Meconium aspiration syndrome
Tracheo-esophageal fistula
Pyloric stenosis
Duodenal atresia
A previously healthy 2-year-old male is brought to the emergency department after experiencing a seizure-like episode. His parents report that he has been healthy with the exception of mild upper respiratory symptoms for the past 24 hours. During the episode, his parents state that he fell down and had rhythmic, jerking movements of his arms and legs. The episode lasted about three minutes. The patient was sleepy when the emergency personnel arrived. Vital signs are temperature 39.2 c (102.5 F), pulse 120/min, and respiratory rate 25/min. The patient is alert and oriented in the emergency department. On examination, there is mild rhinorrhea and the left tympanic membrane is erythematous, bulging, and poorly mobile. The neck is supple. A complete neurological exam is unremarkable. After treating this patient's fever, which of the following is the next best step in the management of this patient?
Lumbar puncture
Discharge home with education
Magnetic resonance imaging of the brain
Admit for further observation
Electroencephalogram
A child has a 2-week history of spiking fevers, which have been as high as 40°C (104°F). She has spindle-shaped swelling of finger joints and complains of upper sternal pain. When she has fever, the parents note a faint salmon-colored rash that resolves with the resolution of the fever. She has had no conjunctivitis or mucositis, but her heart sounds are muffled and she has increased pulsus paradoxus. Which of the following is the most likely diagnosis?
Osteoarthritis
Rheumatic fever
Juvenile rheumatoid arthritis
Toxic synovitis
Septic arthritis
A 4-year-old girl is brought to the office due to seizures that occurred 2 hours ago. This is her first episode. Her parents are also concerned because she is not able to carry on activities that children of her age are expected to do. On examination, there is a red flat lesion covering the left eye area and adjacent facial skin, which does not blanch on pressure, and which the parents say has been present since birth. Other pertinent findings are hemianopia, hemiparesis, and hemisensory disturbances. An x-ray of the skull shows tramline intra-cranial calcifications. What is the most likely diagnosis?
Epilepsy
Sturge-Weber syndrome
Tuberous sclerosis
Neurofibromatosis
Capillary hemangioma
A 3-week-old infant is being evaluated for hematochezia. His mother states that the infant passed stools j that contain both blood and mucus. There were no complications during her pregnancy, and the infant has been otherwise healthy. On physical examination, his temperature is 37.1 C (98.9 F), pulse is 110/min, and respirations are 18/min. He appears well, and his fontanelle is flat and level. Abdominal examination reveals normal active bowel sounds; his abdomen is nontender to palpation and there is no mass. His diaper contains stool that has bright red blood on it with mucus. Which of the following is the most likely explanation of his hematochezia?
Ulcerative colitis
Food allergy-induced colitis
Rectal fissure
Necrotizing enterocolitis
Meckel diverticulum
A 6-year-old girl with acute lymphocytic leukemia (ALL) is admitted to the hospital with a generalized vesicular rash and high fever. She has no previous history of chickenpox and has never received immunization for varicella. Her 4-year-old sister recently recovered from chickenpox that started about 10 days ago. On admission, her temperature is 38.4 C (101.1 F), blood pressure is 94/58 mm Hg, pulse is 80/min, and respirations are 20/min. Which of the following is the most serious complication of varicella that might occur in this patient?
Endocarditis
Arthritis
Pneumonia
Hepatitis
Cellulitis
A 10-year-old child recently had cognitive testing that showed a full scale intelligence quotient of 105. On achievement testing, he performed at the 3rd percentile in reading and at the 50th percentile in math. Of the following, these findings MOST likely represent
Mental retardation
Attention-deficit/hyperactivity disorder
Specific learning disability
Vision impairment
Poor testing conditions for the achievement test
A 9-year-old girl is brought by her sister to her pediatrician with the complaint of severe, intermittent headaches for the past several months, one of which resulted in her going to the ER. The physical examination today, including a careful neurologic examination, is normal. The headache is diffuse, throbbing, lasts several hours, and is not associated with vomiting or other symptoms. The child cannot feel the headaches coming on; they appear on all days of the week; and usually the headaches are gone when she awakens from a nap. The child reports that she is doing well in school, plays clarinet in the school band, and has “lots of friends.” The sister is not sure, but she thinks their father, who lives in another state, may have headaches. The most likely explanation for this girl’s headache is which of the following?
Tensionheadache
Brain tumor
Migraine
Fungal meningitis
Sinusitis
You are evaluating a 10-year-old boy who has intermittent urinary incontinence. Voiding cystourethrography detects a urethral stricture. Of the following, the MOST likely cause of this boy's urethral stricture is
Trauma
Carcinoma
Chronic infection
Congenital narrowing
Intermittent urolithiasis
A 12-year boy is brought to the emergency room by his parents after a several day history of progressive weakness. He has been a healthy child who has met all development milestones and all his immunizations are up to date. He reports that he had an upper respiratory infection 2 weeks ago. On physical examination, his vital signs are labile with a pulse range of 60-100/ min and systolic blood pressure ranging from 80-120 mm Hg. He is alert and oriented. Neurologic examination is impressive for bilateral weakness in the upper and lower extremities. Deep tendon reflexes are absent and sensation is intact. Which of the following is the most likely diagnosis?
Polymyositis
Myasthenia gravis
Transverse myelitis
Viral encephalitis
Guillain-Barré syndrome
James is an 8-year-old boy who recently attended accident and emergency with a swollen left ankle. He had an x-ray and was discharged home and told there was no fracture. He has now developed a dark purple rash on his legs, which does not disappear with a glass pressed on. He was brought back to the department today vomiting, with abdominal pain. His observations and urine dipstick are all within normal limits. What is the most likely diagnosis?
Diabetic ketoacidosis
Henoch–Schönlein purpura
Meningococcal sepsis
Idiopathic thrombocytopenic purpura
Viral gastroenteritis
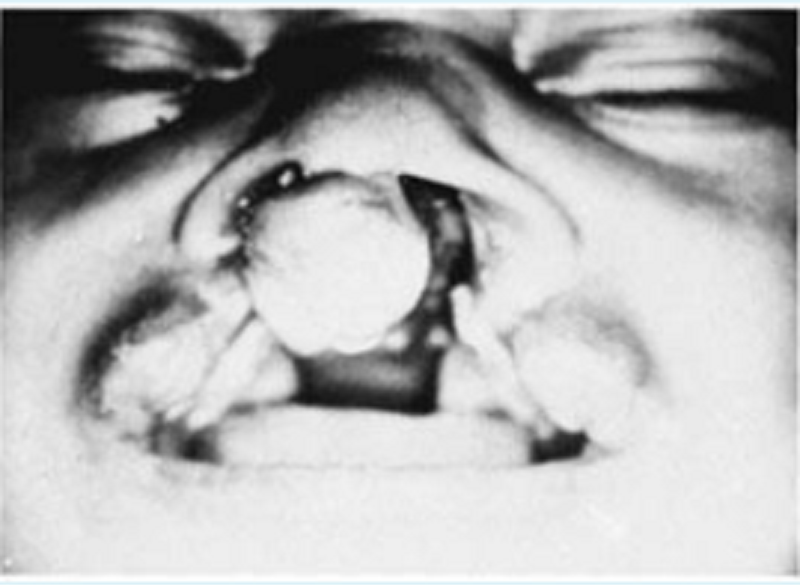
You see the newborn baby shown below for the first time in the nursery. You consult plastic and reconstructive surgeon as well as the hospital’s speech therapist. Understandably, the parents have many questions. Which of the following statements is appropriate anticipatory guidance for this family?
Good anatomic closure will preclude the development of speech defects
The chance that a sibling also would be affected is 1 in 1000
Parenteral alimentation is recommended to prevent aspiration
Recurrent otitis media and hearing loss are likely complications
Surgical closure of the palatal defect should be done before 3 months of age
A 4-year-old child who has Duchenne muscular dystrophy requires operative intervention under general anesthesia for inguinal hernia repair. Of the following, the operative complication that is MORE likely to occur in this child than in a healthy child is
Seizure
Surgical site infection
Malignant hyperthermia
Atlantoaxial rotary subluxation
Corneal damage
A 17-year-old girl comes to the clinic with several weeks of joint pain and rash. The joint pain is most prominent in the hands. She states that the pain is most severe in the morning and tends to improve over the day. She has noted some swelling of her fingers. She has also had a rash on her face that becomes more prominent when she is outdoors. She states that sunlight tends to bother her eyes. On further questioning, she states that she has not felt well for several months. She has had intermittent fever, has been more tired than usual, and has lost weight although she has not been restricting her diet. On physical examination, she looks tired. She has lost 5 lbs since her last visit 1 year ago. She has an erythematous rash on her cheeks. She has several shallow ulcers in her mouth. She has fusiform swelling of her fingers and pain with movement of her fingers. Which of the following is the most likely diagnosis?
Dermatomyositis
Systemic lupus erythematosus (SLE)
Lyme disease
Juvenile rheumatoid arthritis
Rheumatic fever
A mother brings her 2-year-old daughter to the GP on a Monday morning. Over the weekend she became very upset on being told ‘no’. She was screaming and then held her breath, went blue and fainted. She woke up quickly and seemed okay afterwards. However, it has just happened again this morning when she found some scissors and her mother took them away. On this occasion she had a brief generalized convulsion lasting about 10 seconds. What is the most likely explanation?
Vasovagal syncope
Wolff–Parkinson–White syndrome
Absence epilepsy
Reflex anoxic seizures
Breath holding attacks
A 1-day-old boy is evaluated in the nursery for minimal right arm movement. He was born at 41 weeks gestation to a woman with poorly controlled type 1 diabetes mellitus. Attempted vaginal delivery was complicated by shoulder dystocia and became a cesarean section delivery. Family history is positive for obesity in the boy's father and osteoporosis in both grandmothers. Birth weight was 4.5 kg. Examination shows crepitus and irregularity over the right clavicle. Moro reflex is absent on the right. Bilateral biceps and grasp reflexes are intact and symmetric. The infant is plethoric and has excessive fat accumulation in the abdominal and scapular regions. The remainder of the examination is normal. Which of the following is the most significant risk factor for this patient's condition?
Osteogenesis imperfecta
Brachial plexus injury
In utero cerebrovascular accident
Maternal history of diabetes
Family history of osteoporosis
You are evaluating a 12-year-old boy who recently moved to your community. His family history reveals that his father, who is 36 years old, suffers from extremely high blood cholesterol levels (>500 mg/dL [12.9 mmol/L]). The boy's mother states that her husband's brother has the "same problem." Findings on the boy's physical examination are normal. Of the following, the BEST next step for your patient is to
Measure cholesterol and triglyceride concentrations
Order a baseline electrocardiogram
Begin therapy with a lipid-lowering medication
Institute a low-fat diet plan and follow up in 3 months
Obtain a blood sample for genetic testing
A 5-year-old girl presents with a foul-smelling vaginal discharge of 2 weeks' duration. She has a previous history of one urinary tract infection at age 3 years. Of the following, the MOST appropriate next step is
Perianal adhesive tape test
Culture of the discharge for respiratory pathogens
Genital examination using the knee-chest position
Urine for culture and sensitivity
Sitz baths and application of an estrogen cream
A 15-month-old boy is brought into the clinic with a 1-day history of fever, decreased oral intake, and runny nose. His vital signs are within normal limits except for a temperature of 39.5 C (103.1 F). He is active and in no distress. His ears are clear bilaterally. There is a clear nasal discharge. Multiple small (1-2 mm) vesicular lesions are noted on the mucosa of the anterior tonsillar pillars and posterior palate. The rest of his examination is within normal limits. Which of the following is the most likely diagnosis?
Herpangina
Kawasaki disease
Hand-foot-and-mouth disease
Stevens-Johnson syndrome
Aphthous stomatitis
The 3-year-old sister of a newborn baby develops a cough diagnosed as pertussis by nasopharyngeal culture. The mother gives a history of having been immunized as a child. Which of the following is a correct statement regarding this clinical situation?
Erythromycin should be administered to the infant
The 3-year-old sister should be immediately immunized with an additional dose of pertussis vaccine
The mother has no risk of acquiring the disease because she was immunized
Hyperimmune globulin is effective in protecting the infant
The risk to the infant depends on the immune status of the mother
A 14-year-old girl presented to the GP with an enlarged lymph node in her neck. She first noticed it 3 weeks ago and it is increasing in size. She has also had a dry cough, fevers, night sweats and weight loss. She has had a poor appetite over the last 2 weeks, which her mother blames for her weight loss. There is no history of foreign travel or tuberculosis (TB) contacts. A chest x-ray shows a mediastinal mass. What is the most likely diagnosis?
Lymphoma
TB
Leukaemia
Pneumonia
Lung tumour
A 10-month-old infant has poor weight gain, a persistent cough, and a history of several bouts of pneumonitis. The mother describes the child as having very large, foul-smelling stools for months. Which of the following diagnostic maneuvers is likely to result in the correct diagnosis of this child?
CT of the chest
Inspiratory and expiratory chest x-ray
TB skin test
Sweat chloride test
Serum immunoglobulins
A 13-year-old girl is on the ward having a bone marrow transplant for acute leukaemia. She is noted to be profoundly anaemic with haemoglobin 5.9 g/dL and she is due to receive a transfusion of one unit of red blood cells. You are called to see her 5 minutes after starting the transfusion. She has come out in a rash, is looking frightened, with a heart rate of 120 bpm and respiratory rate of 30. As you arrive, you can see she has swollen lips and tongue and her blood pressure is measured as 90/45 mmHg. What is the best initial management step?
Stop the transfusion and return the unit of blood to blood bank
Give IM adrenaline, stop the transfusion, take down the giving set
Repeat a full set of observations as it is likely to be anxiety resulting in the abnormal heart rate, respiratory rate and blood pressure. If still abnormal, stop transfusion
Stop the transfusion, take down the giving set, give IM adrenaline immediately
Stop the transfusion, give IM adrenaline immediately and restart if the reaction settles
An infant is born to a woman who has received very little prenatal care. The mother is anxious, complains of heat intolerance and fatigue, and reports that she has not gained much weight despite having an increased appetite. On examination the mother is tachycardic, has a tremor, and has fullness in her neck and in her eyes. The infant is most likely at risk for development of which of the following?
Third-degree heart block
Thrombocytosis
Constipation
Macrocephaly
Heart failure
A 3-year-old male is brought to the emergency department for evaluation of right neck swelling. His parents noticed a lump on his right neck yesterday, which has since increased in size and is now erythematous and tender. He has been previously healthy except for mild upper respiratory tract symptoms last week. His temperature is 38C (100.4F), pulse is 90/min, and respiratory rate is 25/min. On examination, he is nontoxic appearing. A 5-cm anterior cervical lymph node is palpated on the right side. It is poorly mobile, warm, erythematous, and tender to palpation. There is no fluctuance or induration. What is the most likely organism causing these symptoms?
Francisella tularensis
Epstein-Barr virus
Peptostreptococcus
Nontuberculous mycobacteria
Staphylococcus aureus
A 16-year-old Caucasian girl from the northeastern United States presents for a health supervision visit. She drinks three to four diet sodas a day and describes herself as "a couch potato." She has a history of asthma and had been hospitalized for administration of intravenous methylprednisolone twice in the past year. Physical examination findings are normal. She is at Sexual Maturity Rating 4 and has had normal menses for 3 years. A year ago, she fell while walking and fractured her ulna. You are considering therapy for suspected osteopenia. Of the following, the MOST appropriate therapy for this patient at this time is
Oral calcium and vitamin D supplement
Oral alendronate
Oral estrogen
Intranasal calcitonin
Oral phosphorus supplement
An 18-month-old child is brought into accident and emergency with a 2-day history of vomiting, abdominal pain and fever. Which of the following is an unlikely cause of this clinical picture?
Lower lobe pneumonia with pain referred to the abdomen
NEC
Mesenteric adenitis
Diabetic ketoacidosis
Pyelonephritis
A 16-month-old is taken to the emergency room after falling while learning to walk. The toddler has an enlarging, swollen bruise on his forehead, which is now over two inches across. The parents say that the bruise is noticeably larger than it was when they entered the emergency room an hour earlier. A blood sample is drawn, and the child oozes blood at the puncture site for 25 minutes. Clotting studies on the blood sample show a prolonged PTT and a normal PT. Follow-up studies show very low levels of factor VIII. Which of the following is the most likely diagnosis?
Hemophilia A
Disseminated intravascular coagulation
Hyperhomocysteinemia
Von Willebrand disease
Hemophilia B
A 14-year-old boy has a body mass index that is greater than the 95th percentile for age and an accelerating weight curve. His blood pressure is 135/85 mm Hg. His mother has type 2 diabetes that developed during her first pregnancy, and several paternal relatives also have type 2 diabetes. The family emigrated from the Caribbean when he was a toddler. He has dark velvety thickening of the skin on his neck and under his arms. Of the following, the findings that are MOST supportive of a diagnosis of metabolic syndrome in this young man are
Obesity and maternal history of diabetes
Acanthosis nigricans, obesity
Acanthosis nigricans, hypertension, obesity
Acanthosis nigricans and maternal history of diabete
Hypertension, obesity
A 5-week-old bottle-fed boy presents with persistent and worsening projectile vomiting, poor weight gain, and hypochloremic metabolic alkalosis. Of the following diagnostic modalities, which would most likely reveal the diagnosis?
Serum thyroxine
Barium enema
Ultrasound of abdomen
Testing well water for presence of nitrites
Evaluation of stool for ova and parasites
A 14-year-old African-American girl presents to the ER with a mild fever and severe right-sided thigh pain. She is agitated and requests quick pain relief. Her heart rate is 120/min and blood pressure is 120/70 mmHg. She says that she had a similar episode one year ago and was placed in the hospital for intravenous pain management. Her brother had similar episodes and died of an infection at 10 years of age. Which of the following would you most expect to see on this patient's peripheral blood smear?
Burr cells
Reticulocytosis
Polycythemia
Hypersegmented neutrophils
Iron deficiency
On the day 1 baby check a mother is very concerned about a rash on her baby’s face. Over the right eye, forehead and temple there is a pink-red, flat area of erythema. He is opening the eye, and his eye movements seem intact. The child’s observations and rest of the examination are normal. What should you tell the mother?
This is a capillary haemangioma (stork mark) and is normal; it will fade over the first year or so of life
This is orbital cellulitis and he needs intravenous antibiotics
This is a port wine stain and the baby needs an MRI scan to check for intracranial involvement
This is erythema toxicum which is a normal baby rash and will go away within the first few weeks
This is a strawberry naevus and it may get bigger before it goes away by about 5 years of age
A 6-year-old female is brought to the physician with a rash and joint pains. Her mother reports that she has been previously healthy except for a sore throat a few weeks ago. One week ago, the patient developed pain in her knees. The knee pain resolved after a few days, but now her ankles and wrists are tender. She has also developed a pink rash on her trunk that is non-pruritic. Vital signs are temperature 38.3 c (101 F), pulse 85/min, and respiratory rate 20/min. On examination, there is pain and stiffness during manipulation of the wrists and ankles. A faint, erythematous, centrifugal rash on her trunk and proximal limbs is present. Laboratory studies show: Complete blood count: Hemoglobin 12.5 g/dL, MCHC 32%, MCV 85 fl, Reticulocyte count 0.1%, Platelet count 200,000/mm3, Leukocyte count 6,500/mm3, Neutrophils 56%, Eosinophils 1%, Lymphocytes 33%, Monocytes 10%, C-reactive protein 3.5 mg/dL, Erythrocyte sedimentation rate 38 mm/hr. Which of the following is the most likely diagnosis?
Juvenile rheumatoid arthritis
Acute lymphoblastic leukemia
Fibromyalgia
Rheumatic fever
Systemic lupus erythematosus
A 6-year-old girl is taken to see her GP because she is complaining of knee and elbow pains frequently. Her mother thinks it is worst after her ballet classes and when she gets home from school. She denies stiffness or pain in the mornings. Her mother has been administrating paracetamol several times a week and is worried that this is too much to be giving a child. On examination, the child looks well and has full range of movement of her joints with evidence of hyperextension. There are no swollen joints or effusions present and she is non-tender on examination. What is the most likely diagnosis?
Hypermobile joints
Juvenile idiopathic arthritis (JIA)
Repetitive strain injury
Osteoarthritis
Marfan’s syndrome
A 2-year-old child is admitted to your hospital team. The child’s primary care doctor has been following the child for several days and has noted her to have had high fever, peeling skin, abdominal pain, and a bright red throat. You are concerned because two common pediatric problems that could explain this child’s condition have overlapping presenting signs and symptoms. Which of the following statements comparing these two diseases in your differential is true?
A specific antibiotic therapy is recommended for one of the conditions, but only supportive care is recommended for the other
Only one of the diseases has mucocutaneous and lymph node involvement
Pharyngeal culture aids in the diagnosis of one of the conditions
Neither has cardiac complications
Serologic tests are helpful in diagnosing both
The parents of a 7-month-old boy arrive in your office with the child and a stack of medical records for a second opinion. The boy first started having problems after his circumcision in the nursery when he had prolonged bleeding. Studies were sent at the time for hemophilia, but factor VIII and IX activity were normal. At 2 months he developed bloody diarrhea, which his doctor assumed was a milk protein allergy and changed him to soy; his parents note he still has occasional bloody diarrhea. He has seen a dermatologist several times for eczema, and he has been admitted to the hospital twice for pneumococcal bacteremia. During both admissions, the parents were told that the infant’s platelet count was low, but they have yet to attend the hematology appointment arranged for them. The child’s WBC count and differential were normal. Which of the following is the most likely diagnosis in this child?
Partial thymic hypoplasia
Idiopathic thrombocytopenic purpura
Acute lymphocytic leukemia
Wiskott-Aldrich syndrome
Adenosine deaminase deficiency
A 1-week-old female infant is brought to the office by her 30-year-old African-American mother because she has been "crying a lot." She was born at term. Her mother was diagnosed with gestational diabetes mellitus (GDM) at 24 weeks gestation and had been on insulin injections since. During labor, there was a prolonged second stage due to difficulty in delivering the shoulders. Her Apgar scores were 8 and 10 at 1 and 5 minutes, respectively. Her birth weight is 3.8 kg (8.5 Ib). On examination, the infant is active. On sudden extension of the head, there is extension of all the extremities, except for the left upper extremity. There is crepitus over the left clavicular bone. Which of the following statements is true for this baby?
This is a common outcome with large babies and related to gestational diabetes
This infant has clavicular fracture and should be treated with a surgery
This is a clavicular fracture and the infant should be evaluated for child abuse
This is Erb Duchenne palsy due to difficult shoulder delivery
This infant has clavicular fracture and should be treated with a figure of eight bandage
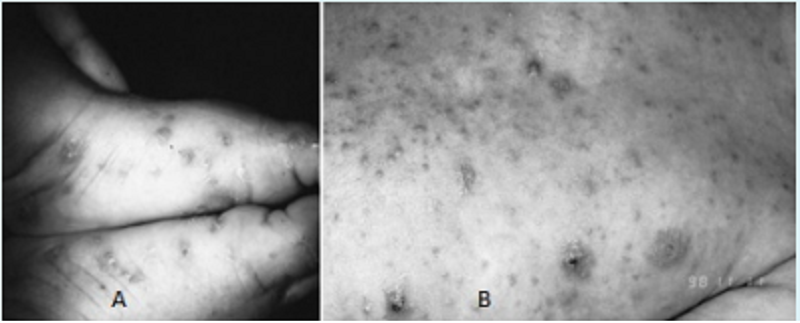
A 2-year-old child (Image A) presents with a 4-day history of a rash limited to the feet and ankles. The papular rash is both pruritic and erythematous. The 3-month-old sibling of this patient (Image B) has similar lesions also involving the head and neck. The most appropriate treatment for this condition includes which of the following?
Emollients
Permethrin
Topical antifungal cream
Hydrocortisone cream
Coal-tar soap
A 5-year-old child develops an earache, but her mother is too busy to take her to the pediatrician. Two weeks later, the child still has not improved and now has a painful, swollen, red area behind the pinna. At this point, the child is taken to the emergency department, where the physician additionally notes the presence of fever and a creamy discharge in the ear canal. Which of the following is the most likely diagnosis?
Acute mastoiditis
Meniere disease
Secretory otitis media
Chronic otitis media
Barotitis media
A 14-year-old male presents with a complaint of soreness, and weakness in his legs for the past day that has slowly spread from his calves to his thighs. He now complains of weakness in his trunk and arms. On examination he appears tired and lays on the examining table. His temperature is 37 C (98.6 F), pulse is 48/min, and respirations are 22/min. Both of his legs are diffusely tender. Deep tendon reflexes are absent in the lower extremities, and sensation is greatly diminished. Which of the following studies is essential for this patient's diagnosis?
Motor nerve conduction test
Stool culture for Campylobacter jejuni
Cerebrospinal fluid studies
Creatinine phosphokinase levels
Muscle biopsy

A 4-year-old girl is noticed by her grandmother to have a limp and a some-what swollen left knee. The parents report that the patient occasionally com- plains of pain in that knee. An ophthalmologic examination reveals findings as depicted in the photograph. Which of the following conditions is most likely to be associated with these findings?
Osgood-Schlatter disease
Legg-Calvé-Perthes disease
Henoch-Schönlein purpura
Slipped capital femoral epiphysis
Juvenile rheumatoid arthritis

A 2-month-old infant is brought to the physician for evaluation of fever. The infant was born at 37 weeks gestation via normal spontaneous vaginal delivery. His mother had an uncomplicated pregnancy and delivery. He has been doing well until this morning when he developed a temperature of 101.5 F (38.6 C). His mother reports that he is still taking his formula well. He has some clear rhinorrhea and intermittent sneezing. His 3-year-old brother had an upper respiratory tract infection one week ago. The patient's chest radiograph is shown below. Which of the following best describes the findings on this patient's chest radiograph?
Right middle lobe infiltrate
Cardiomegaly
Normal cardiothymic silhouette
Right upper lobe infiltrate
Hilar lymphadenopathy
An 8-year-old boy is brought to the office due to headaches and impaired walking. These symptoms started seven days ago, and progressed gradually. He just recently recovered from otitis media that was superimposed on an acute respiratory infection. His past medical history is significant for three episodes of otitis media and one episode of pneumonia. His temperature is 36.7C (98F), blood pressure is 100/60 mm Hg, pulse is 110/min, and respirations are 20/min. Physical examination reveals mild right-sided hemiparesis and a slightly dilated left pupil. The funduscopic examination is normal. Which of the following is the most likely diagnosis?
Toxoplasmosis
Venous thrombosis
Bacterial meningitis
Brain abscess
Arterial thrombosis
A 12-year-old girl was hit in the face by a baseball 15 minutes earlier and has had her mandibular incisors knocked out. Which of the following represents the best plan of action?
The teeth may be transported in tea, juice, or cola
A dental appointment should be made within 48 to 72 hours
Foreign matter adhering to the teeth should be immediately scrubbed off
The teeth should be rinsed in hot water then carefully dried
Avulsed teeth can be transported in the mouth of the parent or a cooperative patient
A 7-day-old female neonate is brought to your office for a 2-day history of jaundice and poor feeding. According to the mother, she has vomited twice but doesn't appear febrile. She is regularly breastfed. Her birth history is unremarkable. On examination, she appears listless, and mild jaundice, along with signs of dehydration, are noted. Her blood pressure is 78/52mm Hg, pulse rate is 150/min, and temperature is 36 C (96 F). Her family history is insignificant. What is the most appropriate next step in the management of this patient?
Obtain blood cultures and lumbar puncture
Obtain Coomb's test and osmotic fragility test
Stop breast feeding
Obtain liver function tests
Obtain peripheral smear and reticulocyte count
A 7-month-old patient presents with a history of 3 days of fever to 104°F, which resolved the same day that an exanthem erupted. The exanthem is prominent on the neck and trunk. It is macular, with discrete lesions 3–5 mm in diameter. Which of the following is the most likely diagnosis?
Scarlet fever
Measles
Rubella
Erythema infectiosum
Roseola infantum
A previously healthy full-term infant has several episodes of duskiness and apnea during the second day of life. Diagnostic considerations should include which of the following?
Congenital heart disease
Hyperglycemia
Idiopathic apnea
Harlequin syndrome
Hemolytic anemia
A 2-week-old infant is brought to the office for a newborn visit. His mother states that the he has been a very slow eater and that he is constipated, not having had a bowel movement in 3 days. On physical examination, the infant has poor muscle tone, an enlarged tongue, an umbilical hernia, an enlarged anterior fontanelle, and hypothermia. He also looks slightly jaundiced, with slightly dry skin and brittle hair. Which of the following is the most likely diagnosis?
Trisomy 21
Turner syndrome
Hurler syndrome
Congenital hypothyroidism
Beckwith-Wiedemann Syndrome
A 16-year-old boy is brought into the emergency department by his friends. He is semicomatose, with a pulse of 60/min and respirations of 6-8/min. His pupils are constricted. Which of the following will most likely be revealed on a urine toxicology screen?
Ethanol intoxication
Opiate intoxication
Tricyclic antidepressant intoxication
Cocaine intoxication
Amphetamine intoxication
On a newborn baby check of an Asian, 36-hour-old baby you note a large bruise coloured area on the buttocks and lower back which seems non-tender. The mother does not know how it got there. He is handling well and the rest of the baby check is unremarkable. What is the most likely explanation?
Neonatal sepsis with disseminated intravascular coagulation
Von Willebrand’s disease
Mongolian blue spot
Idiopathic thrombocytopenic purpura
Non-accidental injury
A 3-year-old boy is brought to the ER with a two-day history of decreased appetite, neck swelling, and irritability. He keeps his head rotated slightly to the right side. He resists passive flexion of the neck and rotation to the left side. Which of the following is the best next step in managing this patient?
Direct laryngoscopy
Botulinum toxin injection
Lumbar puncture
X-ray of the neck
Soft neck collar
A 3-year-old boy is brought to the clinic due to an abdominal mass that his mother noted while she was bathing him. She seems distressed about the matter, and seeks your "expert opinion." The patient does not have any significant past medical history. On examination, he is calm and quiet. A firm abdominal mass is palpated in the left quadrant, which does not cross the midline. The mass is tender on deep palpation, but is not pulsatile Urinalysis reveals a trace amount of blood. What is the most likely diagnosis?
Neuroblastoma
Sarcoma
Lymphoma
Wilms tumor
Pheochromocytoma
An 18-month-old child presents to the emergency center having had a brief, generalized tonic-clonic seizure. He is now postictal and has a temperature of 40C (104F). During the lumbar puncture (which ultimately proves to be normal), he has a large, watery stool that has both blood and mucus in it. Which of the following is the most likely diagnosis in this patient?
Salmonella
Shigella
Rotavirus
Campylobacter
Enterovirus
A 10-year-old child is brought to your office for evaluation of a 1-day history of fever, vomiting, diarrhea, and abdominal pain. His mother states that he has vomited five times, and the emesis has been clear. He has had four episodes of nonbloody diarrhea. He describes his abdominal pain as crampy but cannot localize it to any specific part of his abdomen. He denies any symptoms of dysuria. On physical examination, the child is in no acute distress, his temperature is 99.2°F (37.3°C), heart rate is 102 beats/min, respiratory rate is 26 breaths/min, and blood pressure is 105/70 mm Hg. Results of examination of the head, neck, chest, and heart are normal. His abdomen is soft, and there is no guarding. There is no rebound tenderness. He complains of mild discomfort on deep palpation of his entire abdomen. He has hyperactive bowel sounds on auscultation, and he has no flank tenderness. Of the following, the MOST appropriate next step in the management of this patient is to
Obtain blood for a complete blood count
Obtain serum for electrolyte analysis
Order frontal supine and upright abdomen radiographs
Send the patient home with instructions for supportive care
Administer intravenous fluids

A patient with hair loss is shown below. The lesion does not fluoresce with a Wood lamp and has not responded well to a variety of topical agents. The lesion is boggy, is spreading, and has tiny pinpoint black dots throughout. Which of the following is the most likely diagnosis?
Alopecia areata
Hypothyroidism
Traction alopecia from tight hair braids
Infection with Trichophyton tonsurans
Biotinidasedeficiency
A 5-year-old female child is brought to the emergency department due to fever, chills and abdominal pain. She has been complaining of burning micturition and abdominal pain for the last 2 days. Her temperature is 102 F (38.9C), respirations are 20/min, pulse is 130/min, and blood pressure is 90/60 mmHg. Physical examination reveals costovertebral angle tenderness. Urine analysis shows pyuria, significant bacteriuria, WBC casts, positive nitrite, and esterase. What is the most likely cause of this condition in children?
Vesicoureteral reflux
Ureteral duplication
Wilm's tumor
Renal stones
Hydronephrosis
After being delivered following a benign gestation, a newborn infant is noted to have a platelet count of 35,000/µL, decreased fibrinogen, and elevated fibrin spilt products. On examination you note a large cutaneous hemangioma on the abdomen that is purple and firm. Which of the following anomalies might also be expected in this infant?
Kaposiform hemangioendothelioma
Nevus flammeus
Nevus simplex
PHACE(S) syndrome
Infantile fibrosarcoma
A 12-year-old girl is seen by a pediatrician for a mild case of pneumonia. She is treated with an intramuscular injection of penicillin. About 15 minutes later, she develops extreme itchiness, accompanied by the development of wheals scattered over her chest and extremities. She also begins to wheeze and complain of difficulty breathing. The color of her lips and face remains rosy. Which of the following is the most appropriate first step in management?
Epinephrine injection
Intubation
No specific therapy is needed
IV corticosteroids
Oral corticosteroids
The recent suicide of a well-known high school cheerleader in your community has generated an enormous amount of community concern and media coverage. A girl who was close friends with the deceased makes an appointment and comes in to your office to discuss the event with you. You ask, and she denies suicidal ideation, but she has many questions about suicide. Correct statements about adolescent suicide include which of the following?
The number of attempted suicides is much higher among boys
Girls tend to use more lethal means
Those who are successful have a history of a prior attempt or prior serious suicidal ideation
Inquiry by pediatricians, high school teachers, parents, or friends about suicidal thoughts typically precipitates the act
The number of suicides in adolescents 10 to 19 years of age has decreased significantly since the 1950s
An 8-year-old boy is brought to the emergency department with a head injury. He hit his head on the ground when he fell off his bicycle. He was not wearing a helmet at the time. There was no loss of consciousness. He vomited 2 times after the accident and now complains of a right-sided headache and inability to hear with his right ear. There is no photophobia or diplopia. On physical examination, his blood pressure is 110/72 mm Hg, pulse is 104/min, and respirations are 22/min. He is alert and oriented and responds appropriately to questions. There is a round hematoma on the right side of his head. Bloody drainage is noted from his right ear. Which of the following injury is most consistent with these findings?
Epidural hematoma
Temporal bone fracture
Tympanic membrane perforation
Subdural hematoma
Concussion
A 2-year-old boy is referred to your office for the evaluation of a white eye reflex. His mother suspects a hearing problem because he does not respond when she calls out his name. The physical examination reveals a continuous, machinery murmur over the right 2nd intercostal space and purple lesions on his arms and chest. The initial investigations reveal thrombocytopenia. What is the most likely diagnosis?
Retinoblastoma
Congenital CMV infection
Congenital rubella infection
Sturge Weber syndrome
Congenital Toxoplasma infection
A child is brought to the physician for a routine visit. On examination, the child can name multiple items in the examination room, and can also combine 2 words into a short sentence. His mother estimates that he knows about 200 words. When his mother tries to help him onto the examination table, he says "me do it." Although his mother seems to understand most of what he says, you can only understand about half of his speech. Which of the following is the most likely age of this child?
15 months
12 months
24 months
18 months
36 months
An 11-year-old boy presents with fever and sore throat. A rapid-strep test confirms streptococcal pharyngitis. He is leaving for a summer camp in 2 days. In the past, he has had problem finishing the whole course of antibiotic treatment. Which of the following is the best treatment for his streptococcal pharyngitis?
Penicillin V orally for 5 days
A single dose of procaine penicillin G intramuscularly
A single dose of ceftriaxone intramuscularly
Erythromycin orally for 5 days
A single dose of benzathine penicillin G intramuscularly
A 4-month-old baby is in for a well-child check and routine immunizations. The baby had a fever of 39°C the day he received his 2- month immunizations. The parents have read about the vaccine on the Internet and express their concerns. Which of the following is an absolute contraindication to giving the diphtheria and tetanus toxoids and acellular pertussis (DTaP)?
History of fever >38C after previous vaccination
Current antibiotic therapy
History of local reaction after previous vaccination (redness, soreness, swelling)
Family history of seizures
Encephalopathy within 7 days of administration of previous dose of vaccine
A 3-month-old Jewish infant is brought to the emergency department because of a generalized seizure 1 hour ago. He is lethargic, weighs 2.7kg (61b), and has a doll-like face with fat cheeks, relatively thin extremities, and a protuberant abdomen. His liver is felt 5cm (2in) below the right costal margin. His kidneys are enlarged. His blood sugar level is 40mg/dl. His serum uric acid, total cholesterol, triglycerides and lactic acid levels are elevated. The levels of his liver transaminases are normal. What is the most likely cause of this infant's symptoms?
Deficiency of branching enzyme activity
Acid maltase deficiency
Liver phosphorylase deficiency
Glucose-6-phosphatase deficiency
Deficiency of glycogen debranching enzyme activity
A 14-year-old slightly overweight boy is brought into accident and emergency from a football match where he slipped and fell but was unable to get back up due to pain in his right leg, which is now looking shortened and externally rotated. X-rays show the right femur to be disconnected from the femoral head almost completely at the level of the epiphysis. What is the most appropriate management?
Antibiotics and nil by mouth while waiting for an open reduction operation
Analgesia, nil by mouth until emergency internal fixation can be performed
Analgesia and a hip spica cast
Reassure and mobilize with physiotherapy as tolerated
Analgesia and bed rest with traction until healed
A 6-month-old male infant is brought to the physician's office by his mother due to failure to thrive. According to the mother, the child always regurgitates shortly after feedings, and has even had a few episodes of blood-stained projectile vomiting. During the vomiting episodes, the child tilts his head to the left and arches his back. On examination, the child is afebrile. His abdomen is soft and non-tender to palpation. Laboratory evaluation shows hypochromic microcytic anemia. What is the most appropriate test to confirm the most likely diagnosis of this child?
24-hour esophageal pH monitoring
Chest x-ray
Barium swallow
Technetium (Tc) sulfur colloid gastroesophageal scan
Esophageal manometry
A 15-year-old girl has a round, 1-cm cystic mass in the midline of her neck, at the level of the hyoid bone. The mass is deep to the skin and moves slightly when the patient swallows. When the mass is palpated at the same time that the tongue is pulled, there seems to be a connection between the two. The mass has been present for at least 10 years, but only recently bothered the patient because it became infected. Which of the following is the most likely diagnosis?
Cystic hygroma
Epidermal inclusion cyst
Metastatic thyroid cancer
Thyrogtossal duct cyst
Branchial cleft cyst
A 6-year-old boy had been in his normal state of good health until a few hours prior to presentation to the ER room. His mother reports that he began to have difficulty walking, and she noticed that he was falling and unable to maintain his balance. Which of the following is the most likely cause for his condition?
Agenesis of the corpus callosum
Friedreich ataxia
Drug intoxication
Ataxia telangiectasia
Muscular dystrophy
A neonate is noted to have many abnormalities, a number of which are located in the midline. The infant has cleft lip and cleft palate. His eyes are very small and have fissures of the iris, shallow supraorbital ridges, and slanted palpebral fissures. He is deaf, and the ears are low set and malformed. Each hand has six fingers and a simian crease. Which of the following congenital abnormalities of the brain is particularly likely to be present in this infant?
Anencephaly
Holoprosencephaly
Encephalocele
Hydranencephaly
Porencephaly
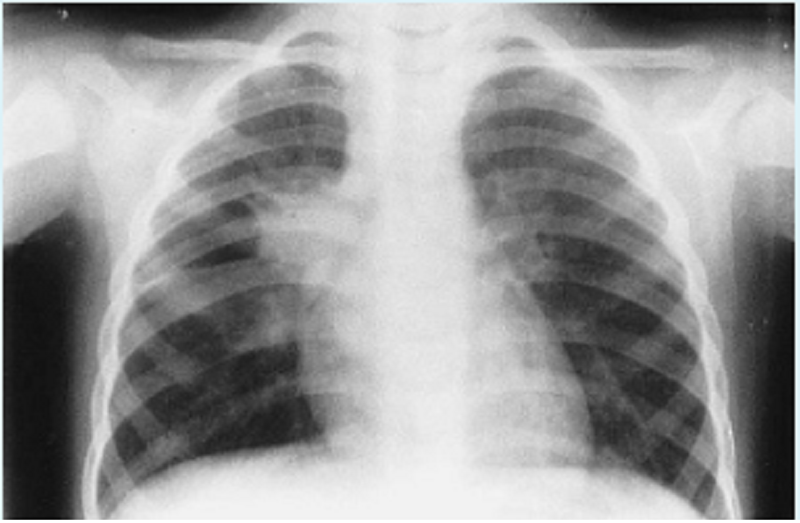
A 3-year-old girl is admitted with the x-ray shown below. The child lives with her parents and a 6-week-old brother. Her grandfather stayed with the family for 2 months before his return to the West Indies 1 month ago. The grandfather had a 3-month history of weight loss, fever, and hemoptysis. Appropriate management of this problem includes which of the following?
Placement of a Mantoux test on the 6-week-old sibling
Isolating the 3-year-old patient for 1 month
Bronchoscopy and culture of washings for all family members
Treating the 3-year-old patient with isoniazid (INH) and rifampin
HIV testing for all family members
A 5-year-old girl presents with a 3-day history of fever, dyspnea, and intermittent joint pain. She has a history of sore throat about 1 month ago. On physical examination, her temperature is 39.6 C (103.2 F), blood pressure is 94/60 mm Hg, pulse is 114/min, and respirations are 22/min. Her knees and elbow joints are swollen and tender to palpation. There is a grade III/VI diastolic murmur best heard at the apex. Multiple fine, pink macules are noted on her trunk. These macules are blanching in the middle. Which of the following is the most likely diagnosis?
Lyme disease
Septic arthritis
Scarlet fever
Rheumatic fever
Juvenile rheumatoid arthritis
Routine examination of an otherwise healthy kindergarten child with a history of asthma reveals a BP of 140/90 mmHg. Which of the following is the most likely cause of the hypertension?
Chronic lung disease
Renal disease
Obesity
Coarctation of the aorta
Theophylline toxicity
A 4-year-old girl was diagnosed of left-side otitis media about 10 days ago and was prescribed oral amoxicillin, 40 mg/kg/day for 7 days. She has since developed bloody diarrhea with mucus, crampy abdominal pain, and fever. On physical examination, her temperature is 39.4 C (102.9 F), pulse is 88/min, and respirations are 16/min. She has normal bowel sounds and is diffusely tender to palpation. Which of the following is the most appropriate initial step in diagnosis?
Evaluation of stool for Clostridium difficile toxins
. Evaluation of stool for rotavirus
Stool Hemoccult test
Barium enema
Stool examination for ova and parasites
A 2-year-old child is brought to the office due to vomiting. He is recovering from an upper respiratory infection, which was treated by his mother with over-the-counter aspirin. On examination he is irritable, lethargic, agitated and uncooperative. His height, weight and head circumference are at the 50th percentile. The pupils are equal and have a sluggish reaction to light. The sclera is non-icteric. The neck is supple and without adenopathy. The abdomen is flat, with normal bowel sounds. The lab findings are as follows: Serum bilirubin Normal, Serum ASAT and ALAT Increased, Serum ammonia Increased, Prothrombin time Prolonged. A CT scan of the brain shows cerebral edema. CSF analysis is normal, except for increased pressure. What is the most likely diagnosis?
Reye syndrome
Viral encephalitis
Sepsis
Aseptic meningitis
Carnitine deficiency
An 8 year old known asthmatic is brought into accident and emergency by ambulance as a ‘blue call’. He has been unwell with an upper respiratory tract infection for the past 2 days. For the past 24 hours his parents have given him 10 puffs of salbutamol every 4 hours, his last dose being 90 minutes ago. The ambulance staff have given him a nebulizer but he remains agitated with a heart rate of 155, respiratory rate of 44 and sub/intercostal recessions and on auscultation there is little air movement heard bilaterally. Saturations in air are 85 per cent. He is started on ‘back to back’ nebulizers with high flow oxygen. How severe is his asthma exacerbation and what other bedside test would support this?
Life-threatening, peak flow <33 per cent expected
Moderate, venous blood pH 4.4, gas PCO2 = 3.1 kPa
Severe, venous blood pH 4.4, gas PCO2 = 3.1 kPa
Severe, peak flow <33 per cent expected
Life-threatening, venous blood pH 4.4, gas PCO2 = 3.1 kPa
A 1-year-old boy is brought to the physician by his parents for evaluation of bruising and blood in his stool. The child has had multiple episodes of otitis media and has been hospitalized twice with pneumonia, but has never had bleeding or easy bruising in the past. He has been eating and drinking well with no vomiting or diarrhea. He is afebrile with a heart rate of 150/min and a blood pressure of 80/40 mmHg. On examination, he is well-developed, well-nourished, and has a fair complexion. There are dry, scaly patches on his cheeks and lower extremities. He also has bruising and purpura on his lower extremities. His diaper contains a small amount of occult blood positive stool, but no fissures are seen on rectal examination. The remainder of the physical examination is unremarkable. Laboratory studies show: Complete blood count: Hemoglobin 11 .5 g/dL, Platelet count 20,000/mm3, Leukocyte count 6,500/mm3, Neutrophils 76%, Eosinophils 1%, Lymphocytes 13%, Monocytes 10%. A peripheral smear reveals a low number of platelets, and the platelets that are seen are small. Which of the following is the most likely cause of his bleeding?
Bone marrow infiltration
Platelet activation and consumption
Platelet antibodies
Impaired platelet production
Nutritional deficiency
An inner city family has been using a neighbor to care for their 3-year-old child while the parents work. The neighbor is diagnosed with pulmonary tuberculosis. PPD test of the 3-year-old is negative. Which of the following is indicated for the 3-year-old?
Isoniazid chemoprophylaxis
No chemoprophylaxis
Ethambutol chemoprophylaxis
Streptomycin chemoprophylaxis
Rifampin chemoprophylaxis
A 3-year-old boy presents to the emergency department following the abrupt onset of coughing and wheezing. You order a chest radiograph for evaluation of a suspected foreign body aspiration. Of the following, the MOST appropriate statement regarding foreign body aspiration is that
The majority of aspirated foreign bodies are located in the larynx or trachea
The classic triad of cough, wheeze, and decreased breath sounds is present in most cases
Toy balloons are a common cause of foreign body aspirations
Most foreign body aspirations present within 24 hours
Nonfood items (eg, coins, pins, pencaps) are the most common items aspirated by infants and toddlers
A 1-day-old male infant has bilious vomiting after every feeding. He hasn't passed any stools yet. He had no prenatal care, and was delivered vaginally at term. He weighs 3kg (6.61b), and his APGAR scores were 6 and 7 at 1 min and 5 min, respectively. On examination, the neonate is hypotonic, he has a flat facial profile, short ears with downfolding ear lobes, a single palmar crease, and a depressed fontanel. There is abdominal distention which is most prominent in the upper abdomen. His abdominal x-rays show gastric and duodenal gas distension with no air distally. What other anomaly can also be expected in this infant?
Meckel's diverticulum
Hirschsprung's disease
Intussusception
Sigmoid volvulus
Meconium plug syndrome
A 12-year-old boy is brought to the emergency department because of severe pain near his left knee. He has sickle cell disease and has been hospitalized previously for sickle cell crisis. Vital signs are notable for persistent fever. Examination of the left lower extremity reveals a normal knee joint with marked tenderness and swelling over the proximal tibia. Laboratory studies show leukocytosis and elevated ESR. Imaging studies confirm the diagnosis of osteomyelitis. Which of the following organisms is the most likely cause of his condition?
Streptococcus pneumoniae
Salmonella species
Pseudomonasspecies
Escherichia coli
Group B streptococcus
A 4-year-old girl is brought to the physician because of a crusted honey-colored erythema resulting from rupture of tiny vesicles and pustules. Her temperature is 37.7 C (102 F). Skin lesions are distributed over the face and extremities. Physical examination reveals enlargement of lymph nodes in the cervical and axillary regions. Which of the following is the most frequent pathogen of this skin infection?
Human herpes virus 7
Streptococcus pyogenes
Staphylococcus aureus
Propionibacterium acnes
Trychophyton fungi
A 14-year-old boy who had a sore throat and fever 2 weeks ago presents to the emergency department still dressed in his football gear from the practice field, where he complained of acute abdominal pain. He exhibits tachypnea, tachycardia, and mild hypotension and complains of intense pain in the left upper quadrant. Of the following, the MOST definitive study to diagnose this child's condition is
Abdominal computed tomography scan
Diagnostic peritoneal lavage
Complete blood count
Abdominal ultrasonography
Partial thromboplastin time
Approximately 19 days after having had a severe sore throat, a 10-year-old girl is taken to a pediatrician because she is complaining that her arms and legs hurt. The mother reports that before the extremity pain began, the child had a rash with irregular boundaries that lasted about a day. Physical examination demonstrates mild fever, as well as swelling and erythema around several large joints. Laboratory studies show an elevated erythrocyte sedimentation rate, and ECG demonstrates a prolonged PR interval. Which of the following is the most likely explanation for these findings?
Antigenic mimicry
Toxin production
Viral infection of myocytes
Parasitic infection of myocytes
Bacterial infection of valves
You are conducting rounds in the newborn nursery with a group of residents. You describe the choices for infant nutrition that might optimize growth and development. Of the following, you are MOST likely to state that:
Term infants require 60 to 80 kcal/kg per day of energy to grow
Preterm infants require less caloric intake per kilogram to grow than do term infants
Term infants whose birthweights are greater than 2,500 g require more energy per kilogram to grow than those whose birthweights are less than 2,500 g
Term infants require 30 to 50 mL/kg per day of fluid intake
Preterm and term infants both require 100 to 120 kcal/kg per day of energy to grow
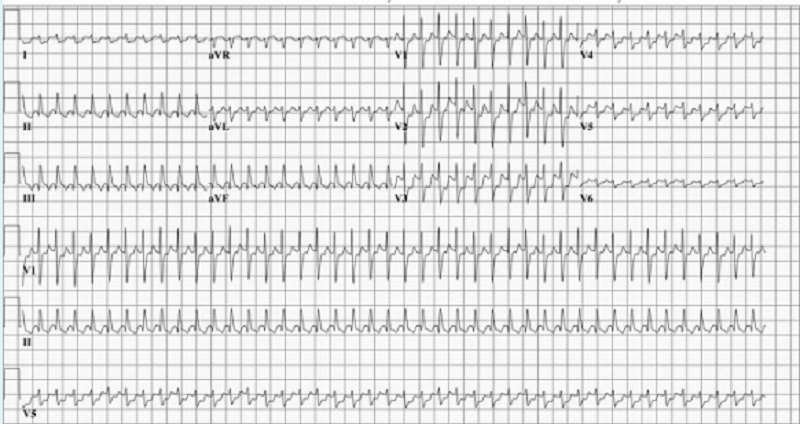
A 3-month-old infant is brought to your office for pallor and listless- ness. Your physical examination reveals tachycardia that is constant and does not vary with crying. He has no hepatomegaly and the lungs are clear. His ECG is shown. Which of the following is the most appropriate initial management of this patient?
DC cardioversion
Precordial thump
Transthoracic pacing of the heart
Carotid massage
Rapid verapamil infusion
You are asked by a colleague to evaluate a 5-year-old boy as a second opinion. He has a history of chronic and recurrent upper respiratory tract infections, several admissions to the hospital for pneumonia, and three surgeries for PE tubes for chronic otitis media. Of note is a right-sided heart on repeated radiographs. Convinced you know the diagnosis based on history alone, you confirm your diagnosis with a biopsy of the nasal mucosa. You expect to find which of the following?
Eosinophilic infiltrate
Bordetella pertussis
Absence of nasal mucous glands
Nasal polyps
Random orientation of cilia
You are examining a 2-day-old term newborn prior to discharge. On physical examination, you note a 5 x 5 cm mass in the right abdomen. The remainder of her physical examination findings are normal. Of the following, the MOST likely diagnosis is
Wilms tumor
Lymphoma
Multicystic dysplastic kidney
Neuroblastoma
Hydrometrocolpos
You are examining a 2-day-old term newborn prior to discharge. On physical examination, you note a 5 x 5 cm mass in the right abdomen. The remainder of her physical examination findings are normal. Of the following, the MOST likely diagnosis is
Wilms tumor
Lymphoma
Multicystic dysplastic kidney
Neuroblastoma
Hydrometrocolpos
A 4-year-old boy from India presents with weakness. His parents note that he has been looking increasingly pale. Hemoglobin electrophoresis demonstrates an abnormal hemoglobin species. Genetic analysis indicates that the patient has the substitution of a valine for a glutamine in the sixth position of the betahemoglobin chain. Which of the following will most likely be seen on his blood smear?
Macrocytic, hypochromic red blood cells
Hypochromic, spherical red blood cells
Hypochromic, sickled red blood cells
Normocytic, hypochromic red blood cells
Normocytic, normochromic red blood cells
A 4-year-old boy from India presents with weakness. His parents note that he has been looking increasingly pale. Hemoglobin electrophoresis demonstrates an abnormal hemoglobin species. Genetic analysis indicates that the patient has the substitution of a valine for a glutamine in the sixth position of the betahemoglobin chain. Which of the following will most likely be seen on his blood smear?
Macrocytic, hypochromic red blood cells
Hypochromic, spherical red blood cells
Hypochromic, sickled red blood cells
Normocytic, hypochromic red blood cells
Normocytic, normochromic red blood cells
A 3 year old is brought to accident and emergency by his parents because he has not been walking for the past day and refuses to stand. He is normally fit and healthy but he did have antibiotics for tonsillitis 2 weeks ago. They do not think he has had any injuries but he attends daycare and something could have happened there. He is up to date with his immunizations and his parents have no concerns with his development. On examination he looks well, is apyrexial, with a heart rate of 120 and respiratory rate of 26 with no bruising. His knees are normal on examination and the hips have a full range of movement except he cries on external rotation of the right hip. There are no deformities seen on x-ray of the hips and knees. After some paracetamol he manages to stand and take a few antalgic steps with encouragement, limping on the right leg. What is the most likely diagnosis?
Osteomyelitis
Growing pains
Reactive arthritis
Non-accidental injury
Septic arthritis
A 3 year old is brought to accident and emergency by his parents because he has not been walking for the past day and refuses to stand. He is normally fit and healthy but he did have antibiotics for tonsillitis 2 weeks ago. They do not think he has had any injuries but he attends daycare and something could have happened there. He is up to date with his immunizations and his parents have no concerns with his development. On examination he looks well, is apyrexial, with a heart rate of 120 and respiratory rate of 26 with no bruising. His knees are normal on examination and the hips have a full range of movement except he cries on external rotation of the right hip. There are no deformities seen on x-ray of the hips and knees. After some paracetamol he manages to stand and take a few antalgic steps with encouragement, limping on the right leg. What is the most likely diagnosis?
Osteomyelitis
Growing pains
Reactive arthritis
Non-accidental injury
Septic arthritis
A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-year-old white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
Persistent pulmonary hypertension of the newborn (PPHN)
Transient tachypnea of the newborn
Meconium aspiration syndrome
Hyaline membrane disease (HMO)
Lntracranial hemorrhage
A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-year-old white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
Persistent pulmonary hypertension of the newborn (PPHN)
Transient tachypnea of the newborn
Meconium aspiration syndrome
Hyaline membrane disease (HMO)
Lntracranial hemorrhage
In the newborn nursery it is noted that a child has uneven gluteal folds. Physical examination of the child's hips reveals that one of them can be easily dislocated posteriorly with a jerk and a "click," and returned to normal position with a "snapping" sound. The family is concerned because a previous child had the same problem. Which of the following is the most likely diagnosis?
Legg-Perthes disease (avascular necrosis of the femoral head)
Developmental dysplasia of the hip
Slipped capital femoral epiphysis
Traumatic delivery
Septic hip
In the newborn nursery it is noted that a child has uneven gluteal folds. Physical examination of the child's hips reveals that one of them can be easily dislocated posteriorly with a jerk and a "click," and returned to normal position with a "snapping" sound. The family is concerned because a previous child had the same problem. Which of the following is the most likely diagnosis?
Legg-Perthes disease (avascular necrosis of the femoral head)
Developmental dysplasia of the hip
Slipped capital femoral epiphysis
Traumatic delivery
Septic hip
A 7-year-old girl presents with a 4-week history of an erythematous rash that involves the eyelids and malar areas and now has occurred at the elbows and knees. Her mother reports that the girl has had a poor appetite, low-grade fevers, muscle aches, and weakness during the past week. Physical examination confirms the rash (Item Q102A). She has difficulty rising from a chair. Other findings on her physical examination are normal. Serum creatine kinase is 677 U/L. Of the following, the test MOST likely to lead to this child's diagnosis is
Molecular testing for fascioscapulohumeral dystrophy
Erythrocyte sedimentation rate
Muscle biopsy
Polymerase chain reaction testing for dystrophin
Serum antinuclear antibody
A 7-year-old girl presents with a 4-week history of an erythematous rash that involves the eyelids and malar areas and now has occurred at the elbows and knees. Her mother reports that the girl has had a poor appetite, low-grade fevers, muscle aches, and weakness during the past week. Physical examination confirms the rash (Item Q102A). She has difficulty rising from a chair. Other findings on her physical examination are normal. Serum creatine kinase is 677 U/L. Of the following, the test MOST likely to lead to this child's diagnosis is
Molecular testing for fascioscapulohumeral dystrophy
Erythrocyte sedimentation rate
Muscle biopsy
Polymerase chain reaction testing for dystrophin
Serum antinuclear antibody
A 3-year-old boy was brought to accident and emergency with his mother. She says he has been limping for a day now and refusing to walk for the last 2 hours. He has had a fever to 39°C which can be brought down with paracetamol. He has had no vomiting, diarrhoea, rash, cough, coryza or injury. He lives with his mother and is her only child. She is currently unemployed and has a background of depression. On examination of the right leg he has a swollen thigh and cries inconsolably when it is touched. It is red and tender. He refuses to allow movement of the hip either passive or active. The left leg is unremarkable on examination. What is the most likely diagnosis?
Septic arthritis
Fractured femur due to non-accidental injury
Perthes’ disease
Juvenile idiopathic arthritis
Fractured femur due to accidental injury
A 3-year-old boy was brought to accident and emergency with his mother. She says he has been limping for a day now and refusing to walk for the last 2 hours. He has had a fever to 39°C which can be brought down with paracetamol. He has had no vomiting, diarrhoea, rash, cough, coryza or injury. He lives with his mother and is her only child. She is currently unemployed and has a background of depression. On examination of the right leg he has a swollen thigh and cries inconsolably when it is touched. It is red and tender. He refuses to allow movement of the hip either passive or active. The left leg is unremarkable on examination. What is the most likely diagnosis?
Septic arthritis
Fractured femur due to non-accidental injury
Perthes’ disease
Juvenile idiopathic arthritis
Fractured femur due to accidental injury
You are called to see a baby who has just been born at 39 weeks’ gestation, as the midwife thinks he is small and should be admitted to the neonatal unit for his care. You review the baby. His weight is 1.8 kg, below the 0.4th centile and his head circumference is 35 cm – 50th centile. He has no dysmorphic features. Which is the most likely cause of this IUGR?
Maternal alcohol use
Maternal smoking
Placental insufficiency
Congenital infection
Chromosomal anomaly
You are called to see a baby who has just been born at 39 weeks’ gestation, as the midwife thinks he is small and should be admitted to the neonatal unit for his care. You review the baby. His weight is 1.8 kg, below the 0.4th centile and his head circumference is 35 cm – 50th centile. He has no dysmorphic features. Which is the most likely cause of this IUGR?
Maternal alcohol use
Maternal smoking
Placental insufficiency
Congenital infection
Chromosomal anomaly
A 3-year-old girl is brought to your office for re-evaluation of a fever that began 6 days ago. Her mother tells you that her daughter's temperature has been as high as 102.2°F (39°C). Her physical examination was unremarkable when you examined her 3 days ago, but today you note injected sclera; cracked, red lips; a strawberry appearance of her tongue; and a swollen, nontender, cervical node. You tell her mother that you believe this is Kawasaki disease. Of the following, the MOST appropriate statement to make to the mother is that
An exercise stress test should be performed as a baseline study
Echocardiography should be performed to evaluate for the presence of coronary aneurysms
Aspirin therapy will be used until the fever subsides
Cardiac involvement may include abnormalities of the coronary arteries or the myocardium
Immediate treatment with intravenous immune globulin will eliminate the chance of coronary involvement
A 3-year-old girl is brought to your office for re-evaluation of a fever that began 6 days ago. Her mother tells you that her daughter's temperature has been as high as 102.2°F (39°C). Her physical examination was unremarkable when you examined her 3 days ago, but today you note injected sclera; cracked, red lips; a strawberry appearance of her tongue; and a swollen, nontender, cervical node. You tell her mother that you believe this is Kawasaki disease. Of the following, the MOST appropriate statement to make to the mother is that
An exercise stress test should be performed as a baseline study
Echocardiography should be performed to evaluate for the presence of coronary aneurysms
Aspirin therapy will be used until the fever subsides
Cardiac involvement may include abnormalities of the coronary arteries or the myocardium
Immediate treatment with intravenous immune globulin will eliminate the chance of coronary involvement
A 16-year-old girl comes to the physician with headache and vision changes for the past month. The headaches are worse in the morning and are associated with nausea. She takes oral isotretinoin for severe acne. Her temperature is 36.7 C, BP is 130/80 mmHg, Pulse is 70/min, and respirations are 15/min. Eye examination shows papilledema and decreased visual acuity. There is no neck stiffness. Motor examination shows 5/5 strength, 2+ deep-tendon reflexes, and a normal plantar response. Sensory examination is unremarkable. Computed tomography scan of the head is within normal limits. Lumbar puncture shows the following: Opening pressure 280 mm H2O, Cerebrospinal fluid glucose 40 mg/dL, Cerebrospinal fluid protein 40 mg/dL, White blood cell 3/mm3. Which of the following is the most likely cause of this patient’s symptoms?
Normal-pressure hydrocephalus
Medication side effect
Classic migraine
Cluster headaches
Multiple sclerosis
A 16-year-old girl comes to the physician with headache and vision changes for the past month. The headaches are worse in the morning and are associated with nausea. She takes oral isotretinoin for severe acne. Her temperature is 36.7 C, BP is 130/80 mmHg, Pulse is 70/min, and respirations are 15/min. Eye examination shows papilledema and decreased visual acuity. There is no neck stiffness. Motor examination shows 5/5 strength, 2+ deep-tendon reflexes, and a normal plantar response. Sensory examination is unremarkable. Computed tomography scan of the head is within normal limits. Lumbar puncture shows the following: Opening pressure 280 mm H2O, Cerebrospinal fluid glucose 40 mg/dL, Cerebrospinal fluid protein 40 mg/dL, White blood cell 3/mm3. Which of the following is the most likely cause of this patient’s symptoms?
Normal-pressure hydrocephalus
Medication side effect
Classic migraine
Cluster headaches
Multiple sclerosis
A 2-year-old boy is hospitalized for severe pneumonia requiring endotracheal intubation and mechanical ventilation. His hemoglobin level is 13.2 mg/dl and his WBC count is 3,200/mm3. The absolute level of CD3- positive lymphocytes is normal but the level of CD 19-positive lymphocytes is very low. This patient would benefit most from which of the following as a maintenance therapy?
Antiretroviral therapy
Intravenous infusion of immune globulin
White blood cell transfusion
Administration of live attenuated vaccines
Enzyme replacement therapy
A 2-year-old boy is hospitalized for severe pneumonia requiring endotracheal intubation and mechanical ventilation. His hemoglobin level is 13.2 mg/dl and his WBC count is 3,200/mm3. The absolute level of CD3- positive lymphocytes is normal but the level of CD 19-positive lymphocytes is very low. This patient would benefit most from which of the following as a maintenance therapy?
Antiretroviral therapy
Intravenous infusion of immune globulin
White blood cell transfusion
Administration of live attenuated vaccines
Enzyme replacement therapy
You are called to examine a 2-day old male infant due to difficulty in feeding. He becomes cyanotic and short of breath when he feeds, but turns pink when he cries. His prenatal, birth and family histories are unremarkable. His vital signs are normal. Chest auscultation is normal. His peripheral pulses are full and symmetric. What is the most likely diagnosis?
Laryngomalacia
Transient tachypnea of the newborn
Choanal atresia
Acyanotic heart disease with left-to-right shunt
Cyanotic heart disease
You are called to examine a 2-day old male infant due to difficulty in feeding. He becomes cyanotic and short of breath when he feeds, but turns pink when he cries. His prenatal, birth and family histories are unremarkable. His vital signs are normal. Chest auscultation is normal. His peripheral pulses are full and symmetric. What is the most likely diagnosis?
Laryngomalacia
Transient tachypnea of the newborn
Choanal atresia
Acyanotic heart disease with left-to-right shunt
Cyanotic heart disease

A 3-day-old infant’s scrotum is shown below. Palpation reveals a tense, fluid-filled area surrounding the right testicle. The scrotum transil luminates well, and the amount of fluid does not vary with mild pressure. Which of the following is the most appropriate approach to this condition?
Request a surgical consultation
Administer prophylactic antibiotics
Incision and drainage
Observe only
Perform a chromosome determination

A 3-day-old infant’s scrotum is shown below. Palpation reveals a tense, fluid-filled area surrounding the right testicle. The scrotum transil luminates well, and the amount of fluid does not vary with mild pressure. Which of the following is the most appropriate approach to this condition?
Request a surgical consultation
Administer prophylactic antibiotics
Incision and drainage
Observe only
Perform a chromosome determination
You are evaluating a very low-birthweight (VLBW) preterm infant who experienced polyuria in the first 72 hours after birth. No diuretics have been prescribed, and there is no glycosuria, hematuria, or obvious anasarca on examination. You collect a urine sample to measure electrolytes and creatinine and simultaneously obtain a blood sample to measure serum electrolytes and creatinine. Of the following, the MOST correct statement regarding sodium handling in the VLBW infant is that
Sodium excretion increases with gestational age
Fractional excretion of sodium is lower than in term infants
Phototherapy increases sodium requirements
Water losses generally exceed sodium losses
Intravenous sodium supplementation is necessary from birth
You are evaluating a very low-birthweight (VLBW) preterm infant who experienced polyuria in the first 72 hours after birth. No diuretics have been prescribed, and there is no glycosuria, hematuria, or obvious anasarca on examination. You collect a urine sample to measure electrolytes and creatinine and simultaneously obtain a blood sample to measure serum electrolytes and creatinine. Of the following, the MOST correct statement regarding sodium handling in the VLBW infant is that
Sodium excretion increases with gestational age
Fractional excretion of sodium is lower than in term infants
Phototherapy increases sodium requirements
Water losses generally exceed sodium losses
Intravenous sodium supplementation is necessary from birth
A 10-year-old boy presents with red discoloration of the urine since the morning. He is healthy and otherwise asymptomatic. He denies dysuria, frequency, urgency, flank, or abdominal pain. His BP is normal. His examination is within normal limits including abdomen and genitourinary system. There is no rash or edema. His urine is pink in color; urinalysis is negative for hemoglobin or protein. No white cells, red cells, or bacteria are noted. Which of the following is the most appropriate next step?
Obtain a recent dietary and drug history
Obtain a renal ultrasound
Obtain antistreptococcal antibodies
Obtain a urine culture
Test for myoglobin in the urine
A 10-year-old boy presents with red discoloration of the urine since the morning. He is healthy and otherwise asymptomatic. He denies dysuria, frequency, urgency, flank, or abdominal pain. His BP is normal. His examination is within normal limits including abdomen and genitourinary system. There is no rash or edema. His urine is pink in color; urinalysis is negative for hemoglobin or protein. No white cells, red cells, or bacteria are noted. Which of the following is the most appropriate next step?
Obtain a recent dietary and drug history
Obtain a renal ultrasound
Obtain antistreptococcal antibodies
Obtain a urine culture
Test for myoglobin in the urine
You are seeing an established patient, a 4-year-old girl brought in by her mother for vaginal itching and irritation. She is toilet trained and has not complained of frequency or urgency, nor has she noted any blood in her urine. Her mother noted she has been afebrile and has not complained of abdominal pain. Mom denies the risk of inappropriate contact; the girl also denies anyone “touching her there.” Your physical examination of the perineum is significant for the lack of foul odor or discharge. You do note some erythema of the vulvar area but no evidence of trauma. Which of the following is the most appropriate course of action?
Refer to pediatric gynecology for removal under anesthesia of a suspected foreign body in the vagina
Treat with an antifungal cream for suspected yeast infection
Swab for gonorrhea and plate on chocolate agar, and send urine for Chlamydia
Counsel mother to stop giving the girl bubble baths, have the girl wear only cotton underwear, and improve hygiene
Refer to social services for suspected physical or sexual abuse
You are seeing an established patient, a 4-year-old girl brought in by her mother for vaginal itching and irritation. She is toilet trained and has not complained of frequency or urgency, nor has she noted any blood in her urine. Her mother noted she has been afebrile and has not complained of abdominal pain. Mom denies the risk of inappropriate contact; the girl also denies anyone “touching her there.” Your physical examination of the perineum is significant for the lack of foul odor or discharge. You do note some erythema of the vulvar area but no evidence of trauma. Which of the following is the most appropriate course of action?
Refer to pediatric gynecology for removal under anesthesia of a suspected foreign body in the vagina
Treat with an antifungal cream for suspected yeast infection
Swab for gonorrhea and plate on chocolate agar, and send urine for Chlamydia
Counsel mother to stop giving the girl bubble baths, have the girl wear only cotton underwear, and improve hygiene
Refer to social services for suspected physical or sexual abuse
A 7 -year-old girl is brought to the clinic by her mother due to a persistent postnasal drip and repeated episodes of a runny nose. In the winter, she experiences several episodes of upper respiratory tract infections, which last for two to three weeks at a time. She snores, and is unable to smell her favorite food. Her immunizations are up-to-date. On examination, she is mildly underweight for her age. She has a runny nose, and her nasal drainage is colorless and stringy. Nasal inspection reveals bilateral nasal polyps, and auscultation of the chest reveals coarse rales. What is the one condition that you would like to rule out in this child?
Leukemia
Nasal septal deviation
Foreign body aspiration
Allergic rhinitis
Cystic fibrosis
A 7 -year-old girl is brought to the clinic by her mother due to a persistent postnasal drip and repeated episodes of a runny nose. In the winter, she experiences several episodes of upper respiratory tract infections, which last for two to three weeks at a time. She snores, and is unable to smell her favorite food. Her immunizations are up-to-date. On examination, she is mildly underweight for her age. She has a runny nose, and her nasal drainage is colorless and stringy. Nasal inspection reveals bilateral nasal polyps, and auscultation of the chest reveals coarse rales. What is the one condition that you would like to rule out in this child?
Leukemia
Nasal septal deviation
Foreign body aspiration
Allergic rhinitis
Cystic fibrosis
A 2-year-old boy is brought to the clinic because of a swelling at the base of his neck on the left side. The family indicates that since he was born, they suspected he had some kind of a mass in his left supraclavicular area and behind the sternomastoid on that same side, but the area felt soft and mushy, was not always evident, and seemed to be painless, so they did nothing about it. Two weeks ago the child had an upper respiratory infection, and within a day or two the mass became larger and quite obvious. On physical examination he indeed has a soft, mushy, ill-defined mass occupying the entire left supraclavicular area and extending into the posterior triangle of the neck. He has no enlarged lymph nodes anywhere, and his spleen and liver are not palpable. Which of the following is the most appropriate next step in the evaluation?
MRI of the neck and chest
Bone marrow biopsy
Panendoscopy under general anesthesia
Multiple percutaneous needle biopsies
Open surgical excisional biopsy
A 2-year-old boy is brought to the clinic because of a swelling at the base of his neck on the left side. The family indicates that since he was born, they suspected he had some kind of a mass in his left supraclavicular area and behind the sternomastoid on that same side, but the area felt soft and mushy, was not always evident, and seemed to be painless, so they did nothing about it. Two weeks ago the child had an upper respiratory infection, and within a day or two the mass became larger and quite obvious. On physical examination he indeed has a soft, mushy, ill-defined mass occupying the entire left supraclavicular area and extending into the posterior triangle of the neck. He has no enlarged lymph nodes anywhere, and his spleen and liver are not palpable. Which of the following is the most appropriate next step in the evaluation?
MRI of the neck and chest
Bone marrow biopsy
Panendoscopy under general anesthesia
Multiple percutaneous needle biopsies
Open surgical excisional biopsy
You are examining a 5-year-old girl who always has had significant daytime wetting and a history of recurrent urinary tract infections. Findings on physical examination are normal except for the presence of a sacral dimple above the gluteal cleft. Her urinalysis reveals a specific gravity of 1.005, pH of 5.5, no blood, no protein, and no white or red blood cells. Magnetic resonance imaging of the spine reveals spinal dysraphism. Of the following, the MOST important next step to determine the cause of this child's primary enuresis is to obtain
Abdominal computed tomography scan
Abdominal ultrasonography
Renal biopsy
Abdominal radiography
Urine culture
You are examining a 5-year-old girl who always has had significant daytime wetting and a history of recurrent urinary tract infections. Findings on physical examination are normal except for the presence of a sacral dimple above the gluteal cleft. Her urinalysis reveals a specific gravity of 1.005, pH of 5.5, no blood, no protein, and no white or red blood cells. Magnetic resonance imaging of the spine reveals spinal dysraphism. Of the following, the MOST important next step to determine the cause of this child's primary enuresis is to obtain
Abdominal computed tomography scan
Abdominal ultrasonography
Renal biopsy
Abdominal radiography
Urine culture
A 25-year-old woman comes to your office for counseling. She says that her husband has cystic fibrosis, and that she has no family history of this disease. They are planning to have a child. She wonders what the probability is for their baby to have cystic fibrosis. Which of the following is your best response in this situation?
Cystic fibrosis is an autosomal recessive disease, so the child has 50% probability of getting the disease
The probability cannot be determined because her carrier status is unknown
Cystic fibrosis is an autosomal dominant disease, so the child will have the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 25% probability of getting the disease
The probability cannot be determined because cystic fibrosis does not follow Mendelian transmission
A 25-year-old woman comes to your office for counseling. She says that her husband has cystic fibrosis, and that she has no family history of this disease. They are planning to have a child. She wonders what the probability is for their baby to have cystic fibrosis. Which of the following is your best response in this situation?
Cystic fibrosis is an autosomal recessive disease, so the child has 50% probability of getting the disease
The probability cannot be determined because her carrier status is unknown
Cystic fibrosis is an autosomal dominant disease, so the child will have the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 25% probability of getting the disease
The probability cannot be determined because cystic fibrosis does not follow Mendelian transmission
A 4-month-old infant boy has gained only 10 ounces since birth. He has failed to gain weight with multiple formula preparations. His stools have been loose and fatty. An older sister had similar symptoms and has been repeatedly hospitalized for failure to thrive and recurrent pulmonary infections. Which of the following is the most likely cause of this patient's gastrointestinal symptoms?
Bacterial overgrowth
Colonic inertia
Gastric hypersecretion
Pancreatic exocrine insufficiency
Achlorhydria
A 4-month-old infant boy has gained only 10 ounces since birth. He has failed to gain weight with multiple formula preparations. His stools have been loose and fatty. An older sister had similar symptoms and has been repeatedly hospitalized for failure to thrive and recurrent pulmonary infections. Which of the following is the most likely cause of this patient's gastrointestinal symptoms?
Bacterial overgrowth
Colonic inertia
Gastric hypersecretion
Pancreatic exocrine insufficiency
Achlorhydria
A 4-year-old boy presents to the emergency department with generalized tonic-clonic seizures. On physical examination, the child is noted to be lethargic. His temperature is 37.4 C (99.3 F), blood pressure is 100/60 mm Hg, pulse is 72/min, and respirations are 16/min. His oral mucosa is moist, and there is no peripheral edema. Laboratory tests show: Blood: Sodium 120 mEq/L, Potassium 4.2 mEq/L, Chloride 96 mEq/L, Bicarbonate 20 mEq/L, Blood urea nitrogen 9.6 mg/dL, Creatinine 0.4 mg/dL, Glucose 88 mg/dL, Urine: Sodium 55 mEq/L, Potassium 16 mEq/L, Osmolality 530 mOsmol/kg. Which of the following is the most likely diagnosis?
Acute renal failure
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
Congestive heart failure
Addison disease
Hyponatreraic dehydration
A 4-year-old boy presents to the emergency department with generalized tonic-clonic seizures. On physical examination, the child is noted to be lethargic. His temperature is 37.4 C (99.3 F), blood pressure is 100/60 mm Hg, pulse is 72/min, and respirations are 16/min. His oral mucosa is moist, and there is no peripheral edema. Laboratory tests show: Blood: Sodium 120 mEq/L, Potassium 4.2 mEq/L, Chloride 96 mEq/L, Bicarbonate 20 mEq/L, Blood urea nitrogen 9.6 mg/dL, Creatinine 0.4 mg/dL, Glucose 88 mg/dL, Urine: Sodium 55 mEq/L, Potassium 16 mEq/L, Osmolality 530 mOsmol/kg. Which of the following is the most likely diagnosis?
Acute renal failure
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
Congestive heart failure
Addison disease
Hyponatreraic dehydration
A 10-year-old boy is brought to clinic because of increasing weakness and dyspnea over the past 6 months. He has been previously healthy and is on no medications. There is no significant family history of illness. On examination, he appears pale. His hematocrit is 20%, mean corpuscular volume (MCV) is 60/mm3, and iron level is normal. Smear reveals basophilic stippling. Hemoglobin electrophoresis is consistent with the absence of one beta-globin gene. Which of the following is the most likely diagnosis?
EUiptocytosis
Sickle cell disease
Porphyria
Thalassemia
Hemoglobin S-C disease
A 10-year-old boy is brought to clinic because of increasing weakness and dyspnea over the past 6 months. He has been previously healthy and is on no medications. There is no significant family history of illness. On examination, he appears pale. His hematocrit is 20%, mean corpuscular volume (MCV) is 60/mm3, and iron level is normal. Smear reveals basophilic stippling. Hemoglobin electrophoresis is consistent with the absence of one beta-globin gene. Which of the following is the most likely diagnosis?
EUiptocytosis
Sickle cell disease
Porphyria
Thalassemia
Hemoglobin S-C disease
Parents bring their 17-year-old son to the emergency department due to his strange behavior at times during the past few weeks. The boy is normally polite and soft-spoken, but he has recently become irritable, impatient, and rude. His parents initially dismissed his behavior as a “phase” with the expectatioin that he would grow out of it. However, they became very concerned on discovering that he had stolen money from their wallets and was sleeping erratically. When questioned by his father about his strange behavior, the boy responsed, “I’m on a secret mission. The king of Norway has sent me here to spy on the US government.” His temperature is 36.6 C, BP is 144/94 mmHg, pulse is 118/min, and respirations are 18/min. On physical examination, the patient appears to be irritated. He is sweating profusely and his pupils are dilated. He is observed in the emergency department for several hours, his condition improves, and he is discharged to the care of his parents. Which of the following is the most likely diagnosis?
Manic episode
Brief psychotic disorder
Amphetamine intoxication
Heroin withdrawal
Anticholinergic poisoning
Parents bring their 17-year-old son to the emergency department due to his strange behavior at times during the past few weeks. The boy is normally polite and soft-spoken, but he has recently become irritable, impatient, and rude. His parents initially dismissed his behavior as a “phase” with the expectatioin that he would grow out of it. However, they became very concerned on discovering that he had stolen money from their wallets and was sleeping erratically. When questioned by his father about his strange behavior, the boy responsed, “I’m on a secret mission. The king of Norway has sent me here to spy on the US government.” His temperature is 36.6 C, BP is 144/94 mmHg, pulse is 118/min, and respirations are 18/min. On physical examination, the patient appears to be irritated. He is sweating profusely and his pupils are dilated. He is observed in the emergency department for several hours, his condition improves, and he is discharged to the care of his parents. Which of the following is the most likely diagnosis?
Manic episode
Brief psychotic disorder
Amphetamine intoxication
Heroin withdrawal
Anticholinergic poisoning
A 5-year-old boy is brought to an emergency room because of a painful, swollen knee joint. The boy had fallen while playing, and the joint had subsequently begun to swell. The mother reports that the boy was known to have hemophilia B. Replacement of which of the following is indicated?
Factor IX
Factor VII
Factor S
Factor VIII
Factor C
A 5-year-old boy is brought to an emergency room because of a painful, swollen knee joint. The boy had fallen while playing, and the joint had subsequently begun to swell. The mother reports that the boy was known to have hemophilia B. Replacement of which of the following is indicated?
Factor IX
Factor VII
Factor S
Factor VIII
Factor C
A 2-month-old exclusively breast-fed infant presents to your office because his mother thinks that he is irritable. His mother reports that the infant has been passing loose stools and cries when he has a bowel movement. He is generally happy at other times. Physical examination demonstrates a healthy, afebrile, vigorous infant who has normal skin color. Cardiac, pulmonary, and abdominal examination findings are all normal. Anal inspection demonstrates no fissures. A stool specimen has reddish flecks, and the guaiac test is positive. Of the following, the BEST next step is to
Send stool for Clostridium difficile toxin testing
Obtain an upper gastrointestinal radiography series
Begin therapy with oral amoxicillin
Remove milk products from the maternal diet
Institute a trial of lansoprazole
A 2-month-old exclusively breast-fed infant presents to your office because his mother thinks that he is irritable. His mother reports that the infant has been passing loose stools and cries when he has a bowel movement. He is generally happy at other times. Physical examination demonstrates a healthy, afebrile, vigorous infant who has normal skin color. Cardiac, pulmonary, and abdominal examination findings are all normal. Anal inspection demonstrates no fissures. A stool specimen has reddish flecks, and the guaiac test is positive. Of the following, the BEST next step is to
Send stool for Clostridium difficile toxin testing
Obtain an upper gastrointestinal radiography series
Begin therapy with oral amoxicillin
Remove milk products from the maternal diet
Institute a trial of lansoprazole
A 2-year-old girl is brought to your clinic because her mother noticed blood in her underwear that morning. She has otherwise been doing well, and she recently has been toilet trained. Findings on the physical examination, including the hymen and external genitalia, are normal. There is a small amount of purulent, bloody discharge at the vaginal introitus. Of the following, the MOST likely cause of her bleeding I
Penetrating trauma
Sarcoma botryoides
Precocious puberty
Vaginal foreign body
Urethral prolapse
A 2-year-old girl is brought to your clinic because her mother noticed blood in her underwear that morning. She has otherwise been doing well, and she recently has been toilet trained. Findings on the physical examination, including the hymen and external genitalia, are normal. There is a small amount of purulent, bloody discharge at the vaginal introitus. Of the following, the MOST likely cause of her bleeding I
Penetrating trauma
Sarcoma botryoides
Precocious puberty
Vaginal foreign body
Urethral prolapse
A 16-year-old girl presents with a history of primary amenorrhea. On examination, short stature and a short neck with a low posterior hairline are noted. Chromosomal analysis most likely would reveal which of the following?
Fragile X
Trisomy 21
XXY
45,XO
Trisomy 18
A 16-year-old girl presents with a history of primary amenorrhea. On examination, short stature and a short neck with a low posterior hairline are noted. Chromosomal analysis most likely would reveal which of the following?
Fragile X
Trisomy 21
XXY
45,XO
Trisomy 18
A 10-year-old girl with Graves’ disease attends her GP with worsening of her symptoms. She was well controlled on carbimazole and has had relatively few symptoms for the past 6 months. She now has sweats, weight loss, diarrhoea and tremors which are affecting her school performance. What is the next management step?
Stop carbimazole and start propranolol
Referral for thyroidectomy
Radioisotope therapy
Review in 3 months
Optimize carbimazole dose and add propanolol
A 10-year-old girl with Graves’ disease attends her GP with worsening of her symptoms. She was well controlled on carbimazole and has had relatively few symptoms for the past 6 months. She now has sweats, weight loss, diarrhoea and tremors which are affecting her school performance. What is the next management step?
Stop carbimazole and start propranolol
Referral for thyroidectomy
Radioisotope therapy
Review in 3 months
Optimize carbimazole dose and add propanolol
A 6-month-old infant is brought to the clinic for the evaluation of sudden episodes of jerky movements of the neck, arms, and legs onto the trunk for past month. These episodes occur in clusters, last for a few minutes, and are often preceded by a cry. Her development has been normal. Her vital signs are normal. She is at 50th percentile for height, weight and head circumference. She has multiple small 1-2 cm oval irregular hypopigmented macules on her trunk and extremities. A head CT scan reveals cortical tubers in the cerebral cortex and multiple subependymal nodules in the lateral ventricles. Her EEG shows "hypsarrhythmia." What is the best medication for this patient's seizure?
Phenobarbital
Carbamazepine
Ethosuximide
ACTH
Vigabatrin
A 6-month-old infant is brought to the clinic for the evaluation of sudden episodes of jerky movements of the neck, arms, and legs onto the trunk for past month. These episodes occur in clusters, last for a few minutes, and are often preceded by a cry. Her development has been normal. Her vital signs are normal. She is at 50th percentile for height, weight and head circumference. She has multiple small 1-2 cm oval irregular hypopigmented macules on her trunk and extremities. A head CT scan reveals cortical tubers in the cerebral cortex and multiple subependymal nodules in the lateral ventricles. Her EEG shows "hypsarrhythmia." What is the best medication for this patient's seizure?
Phenobarbital
Carbamazepine
Ethosuximide
ACTH
Vigabatrin
A 12-month-old infant presents with bilious vomiting and abdominal distention for 10 hours. His mother states that the infant has been constipated since birth and failed to pass meconium during the first 48 hours of life. On examination, he is very irritable. His length and weight are both below the 5th percentile according to his age. His abdomen is moderately distended. After a digital rectal examination, a fair amount of stool ejects out from the anus. Which of the following is the most likely diagnosis?
Malrotation
Duodenal atresia
Hirschsprung disease
Intussusception
Pyloric stenosis
A 12-month-old infant presents with bilious vomiting and abdominal distention for 10 hours. His mother states that the infant has been constipated since birth and failed to pass meconium during the first 48 hours of life. On examination, he is very irritable. His length and weight are both below the 5th percentile according to his age. His abdomen is moderately distended. After a digital rectal examination, a fair amount of stool ejects out from the anus. Which of the following is the most likely diagnosis?
Malrotation
Duodenal atresia
Hirschsprung disease
Intussusception
Pyloric stenosis
A term neonate is small for date and has a small head. Further physical examination of the infant demonstrates small eyes with short palpebral fissures, a flattened nose, and abnormal palmar creases. With which of the following maternal conditions is this presentation most likely associated?
Hypothyroidism
Diabetes mellitus
Cocaine abuse
Alcohol abuse
Cirrhosis
A term neonate is small for date and has a small head. Further physical examination of the infant demonstrates small eyes with short palpebral fissures, a flattened nose, and abnormal palmar creases. With which of the following maternal conditions is this presentation most likely associated?
Hypothyroidism
Diabetes mellitus
Cocaine abuse
Alcohol abuse
Cirrhosis
A 1-year-old child presents with failure to thrive, frequent large voids of dilute urine, excessive thirst, and three episodes of dehydration not associated with vomiting or diarrhea. Over the years, other family members reportedly have had similar histories. Which of the following is the most likely diagnosis?
Diabetes mellitus
Water intoxication
Nephrotic syndrome
Diabetes insipidus
Child abuse
A 1-year-old child presents with failure to thrive, frequent large voids of dilute urine, excessive thirst, and three episodes of dehydration not associated with vomiting or diarrhea. Over the years, other family members reportedly have had similar histories. Which of the following is the most likely diagnosis?
Diabetes mellitus
Water intoxication
Nephrotic syndrome
Diabetes insipidus
Child abuse
You see a 7-day-old baby boy the day that his newborn screening test is reported to show a low thyroxine concentration of 7.8 mcg/dL (100.4 nmol/L) and a thyroid-stimulating hormone concentration of 25 mcU/mL. The baby had a birthweight of 3,000 g and now weighs 3,100 g and is 48.3 cm long. He looks healthy, and the thyroid is not palpable. The mother reports that she isbreastfeeding, and the baby seems to be feeding well. He is her first child. The mother tells you that she takes thyroid hormone for an underactive thyroid and has needed to take calcium and vitamin D since she was a small child "to keep her calcium up." You look at her more closely and realize that she is plump, quite short (perhaps 4 ft 10 in), has a round face, and has short stubby fingers. She says that her mother also had short stature and similar problems. She has one brother who has similar problems and a sister who is 5 ft 6 in and does not have a problem with her calcium. Of the following, this baby and his mother MOST likely have
McCune Albright syndrome
Pseudohypoparathyroidism
Noonan syndrome
Vitamin D resistance
Multiple endocrine autoimmune syndrome
You see a 7-day-old baby boy the day that his newborn screening test is reported to show a low thyroxine concentration of 7.8 mcg/dL (100.4 nmol/L) and a thyroid-stimulating hormone concentration of 25 mcU/mL. The baby had a birthweight of 3,000 g and now weighs 3,100 g and is 48.3 cm long. He looks healthy, and the thyroid is not palpable. The mother reports that she isbreastfeeding, and the baby seems to be feeding well. He is her first child. The mother tells you that she takes thyroid hormone for an underactive thyroid and has needed to take calcium and vitamin D since she was a small child "to keep her calcium up." You look at her more closely and realize that she is plump, quite short (perhaps 4 ft 10 in), has a round face, and has short stubby fingers. She says that her mother also had short stature and similar problems. She has one brother who has similar problems and a sister who is 5 ft 6 in and does not have a problem with her calcium. Of the following, this baby and his mother MOST likely have
McCune Albright syndrome
Pseudohypoparathyroidism
Noonan syndrome
Vitamin D resistance
Multiple endocrine autoimmune syndrome
An adolescent male presents with a hypopigmented eruption composed of multiple oval macules arrayed across the upper trunk in a yoke distribution. Of the following, the PREFERRED management course consists of
Topical application of moderately potent corticosteroid
Avoidance of the offending allergen
Topical application of selenium sulfide
Administration of oral griseofulvin
Application of psoralen followed by ultraviolet radiation
An adolescent male presents with a hypopigmented eruption composed of multiple oval macules arrayed across the upper trunk in a yoke distribution. Of the following, the PREFERRED management course consists of
Topical application of moderately potent corticosteroid
Avoidance of the offending allergen
Topical application of selenium sulfide
Administration of oral griseofulvin
Application of psoralen followed by ultraviolet radiation
A previously healthy 18-month-old male comes to the physician for evaluation of fever. His mother reports that he has had a fever ranging from 1 02.2 F (39.0 c) to 104.0 F (40.0 C) for the past five days. He has also become increasingly irritable with decreased appetite. His mother reports that he does continue to take some liquids. There are no known sick contacts. On examination, the infant's temperature is 102.5 F (39.2 C), pulse is 120/min, and respiratory rate is 20/min. He is irritable during the examination. There is conjunctival erythema bilaterally, with serous drainage from both eyes. His oropharynx is erythematous and his lips are fissured. There is a 2 cm anterior cervical lymph node palpable on the right side. His neck is otherwise supple and he is able to flex his chin to his chest without difficulty. There is mild abdominal tenderness to palpation. His hands and feet are slightly erythematous and edematous and there is a maculopapular rash on the trunk. Which of the following is the most likely diagnosis?
Scarlet fever
Staphylococcal scalded skin syndrome
Toxic shock syndrome
Kawasaki disease
Rocky Mountain spotted fever
A previously healthy 18-month-old male comes to the physician for evaluation of fever. His mother reports that he has had a fever ranging from 1 02.2 F (39.0 c) to 104.0 F (40.0 C) for the past five days. He has also become increasingly irritable with decreased appetite. His mother reports that he does continue to take some liquids. There are no known sick contacts. On examination, the infant's temperature is 102.5 F (39.2 C), pulse is 120/min, and respiratory rate is 20/min. He is irritable during the examination. There is conjunctival erythema bilaterally, with serous drainage from both eyes. His oropharynx is erythematous and his lips are fissured. There is a 2 cm anterior cervical lymph node palpable on the right side. His neck is otherwise supple and he is able to flex his chin to his chest without difficulty. There is mild abdominal tenderness to palpation. His hands and feet are slightly erythematous and edematous and there is a maculopapular rash on the trunk. Which of the following is the most likely diagnosis?
Scarlet fever
Staphylococcal scalded skin syndrome
Toxic shock syndrome
Kawasaki disease
Rocky Mountain spotted fever
During a well-child visit, the grandmother of an 18-month-old patient is concerned because the child’s feet turn inward. She first noticed this when her grandson began to walk. It does not seem to bother the child. On examining his gait, his knees point forward and his feet turn inward. Which of the following is the most likely cause of this condition?
Adducted great toe
Legg-Calvé-Perthes disease
Femoral anteversion
Metatarsus adductus
Medial tibial torsion
During a well-child visit, the grandmother of an 18-month-old patient is concerned because the child’s feet turn inward. She first noticed this when her grandson began to walk. It does not seem to bother the child. On examining his gait, his knees point forward and his feet turn inward. Which of the following is the most likely cause of this condition?
Adducted great toe
Legg-Calvé-Perthes disease
Femoral anteversion
Metatarsus adductus
Medial tibial torsion
A 6-month-old child was noted to be normal at birth, but over the ensuing months you have been somewhat concerned about his slowish weight gain and his mild delay in achieving developmental milestones. The family calls you urgently at 7:00 AM noting that their child seems unable to move the right side of his body. Which of the following conditions might explain this child’s condition?
Histidinemia
Maple syrup urine disease
Phenylketonuria
Homocystinuria
Cystathioninuria
A 6-month-old child was noted to be normal at birth, but over the ensuing months you have been somewhat concerned about his slowish weight gain and his mild delay in achieving developmental milestones. The family calls you urgently at 7:00 AM noting that their child seems unable to move the right side of his body. Which of the following conditions might explain this child’s condition?
Histidinemia
Maple syrup urine disease
Phenylketonuria
Homocystinuria
Cystathioninuria
A 20-month-old presents to the office with a 2-day history of a harsh, barking cough. His mother states that the cough sounds like a seal. She also states he has not had any fever, although he had a runny nose earlier in the week. On examination, he is notably hoarse with inspiratory stridor. He is not drooling and is sitting on his mother's lap comfortably. The rest of his examination is within normal limits. Which of the following is the most likely diagnosis?
Acute laryngotracheobronchitis
Aspiration of foreign body in the upper respiratory tract
Subglottic stenosis
Epiglottitis
Laryngomalacia
A 20-month-old presents to the office with a 2-day history of a harsh, barking cough. His mother states that the cough sounds like a seal. She also states he has not had any fever, although he had a runny nose earlier in the week. On examination, he is notably hoarse with inspiratory stridor. He is not drooling and is sitting on his mother's lap comfortably. The rest of his examination is within normal limits. Which of the following is the most likely diagnosis?
Acute laryngotracheobronchitis
Aspiration of foreign body in the upper respiratory tract
Subglottic stenosis
Epiglottitis
Laryngomalacia
You are asked to see a term infant in the newborn nursery at 8 hours of age and consider her transfer to the neonatal intensive care unit. The problems and findings reported to you include: poor feeding, emesis, temperature instability (core temperature of 96°F [35.5°C]), hypoglycemia (whole blood glucose concentration of 25 mg/dL [1.4 mmol/L]), and polycythemia (hematocrit of 70% [0.70]). Of the following, the physical finding that is MOST likely to accompany these problems is
Iris coloboma of the right eye
Birthweight of 1,800 g
A tuft of hair over the sacral region
Isolated cleft of the hard palate
Café au lait macule on the left leg
You are asked to see a term infant in the newborn nursery at 8 hours of age and consider her transfer to the neonatal intensive care unit. The problems and findings reported to you include: poor feeding, emesis, temperature instability (core temperature of 96°F [35.5°C]), hypoglycemia (whole blood glucose concentration of 25 mg/dL [1.4 mmol/L]), and polycythemia (hematocrit of 70% [0.70]). Of the following, the physical finding that is MOST likely to accompany these problems is
Iris coloboma of the right eye
Birthweight of 1,800 g
A tuft of hair over the sacral region
Isolated cleft of the hard palate
Café au lait macule on the left leg
A 3-year-old boy is brought to the emergency department three hours after having a seizure. He has been having severe diarrhea for the last three days. His mother recently read about the importance of maintaining adequate hydration during diarrhea, so she had been giving him a lot of milk mixed with water. On examination, his vital signs are stable and mucus membranes are moist. Initial lab results are: Hb 13 g/dl, WBC 6,000/mm3, Platelets 300,000/mm3, Blood Glucose 98 mg/dl, Serum Na 120 mEq/L, Serum K 3.4 mEq/L, Chloride 92 mEq/L, BUN 22 mg/dl, Creatinine 1.2 mg/dl. What is the most likely cause of this patient's seizure?
Severe dehydration
Sepsis
Acute renal failure
SIADH
Water intoxication
A 3-year-old boy is brought to the emergency department three hours after having a seizure. He has been having severe diarrhea for the last three days. His mother recently read about the importance of maintaining adequate hydration during diarrhea, so she had been giving him a lot of milk mixed with water. On examination, his vital signs are stable and mucus membranes are moist. Initial lab results are: Hb 13 g/dl, WBC 6,000/mm3, Platelets 300,000/mm3, Blood Glucose 98 mg/dl, Serum Na 120 mEq/L, Serum K 3.4 mEq/L, Chloride 92 mEq/L, BUN 22 mg/dl, Creatinine 1.2 mg/dl. What is the most likely cause of this patient's seizure?
Severe dehydration
Sepsis
Acute renal failure
SIADH
Water intoxication
A 12-year-old, previously healthy girl presents to her physician with a chief complaint of early morning headaches. She states that these headaches wake her up from sleep 2-3 days a week. She also complains of some vomiting associated with the headaches. The headaches have been getting progressively worse for the past 2 months. She denies any photophobia, dizziness, or blurred vision. There is no history of a recent respiratory infection, runny nose, or cough. There is no history of recent trauma. In the office, her vital signs are within normal limits. Her examination shows pupils that are equal, round, and reactive, with no maxillary or frontal sinus tenderness. Her tympanic membranes are clear and intact. Her neck is supple with full range of motion. Neurologic examination shows a positive Romberg sign. Which of the following tests would most likely confirm the diagnosis?
Plain film of the skull
CT of the brain
MRI of the brain
Spinal tap
Sinus x-ray film
A 12-year-old, previously healthy girl presents to her physician with a chief complaint of early morning headaches. She states that these headaches wake her up from sleep 2-3 days a week. She also complains of some vomiting associated with the headaches. The headaches have been getting progressively worse for the past 2 months. She denies any photophobia, dizziness, or blurred vision. There is no history of a recent respiratory infection, runny nose, or cough. There is no history of recent trauma. In the office, her vital signs are within normal limits. Her examination shows pupils that are equal, round, and reactive, with no maxillary or frontal sinus tenderness. Her tympanic membranes are clear and intact. Her neck is supple with full range of motion. Neurologic examination shows a positive Romberg sign. Which of the following tests would most likely confirm the diagnosis?
Plain film of the skull
CT of the brain
MRI of the brain
Spinal tap
Sinus x-ray film
While making rounds in the newborn nursery, the nurses ask you to examine a 2-day-old infant who is not feeding well. The nurse reports that the infant is irritable, is not sleeping well, and has had several episodes of vomiting and loose stools today. A review of the maternal history reveals that she had poor prenatal care and the pregnancy was complicated by intrauterine growth restriction. On examination, the infant is diaphoretic and has a high-pitched cry. The infant is also noted to have occasional sneezing and is mildly tachypneic. No dysmorphic features are noted and the remainder of the examination is unremarkable. This infant's symptoms are most likely caused by prenatal exposure to which of the following?
Alcohol
Phenytoin
Heroin
Cocaine
Valproic acid
While making rounds in the newborn nursery, the nurses ask you to examine a 2-day-old infant who is not feeding well. The nurse reports that the infant is irritable, is not sleeping well, and has had several episodes of vomiting and loose stools today. A review of the maternal history reveals that she had poor prenatal care and the pregnancy was complicated by intrauterine growth restriction. On examination, the infant is diaphoretic and has a high-pitched cry. The infant is also noted to have occasional sneezing and is mildly tachypneic. No dysmorphic features are noted and the remainder of the examination is unremarkable. This infant's symptoms are most likely caused by prenatal exposure to which of the following?
Alcohol
Phenytoin
Heroin
Cocaine
Valproic acid
A sexually active adolescent male presents with the primary complaint of pubic and perianal pruritus. Careful examination reveals pubic or "crab" lice infestation. Of the following, the MOST characteristic feature of this infestation is that the lice:
Lay viable eggs that may hatch up to 7 days after being attached to a hair shaft
Only infest pubic and perianal regions
Rarely infest African-American patients
May survive for 36 hours without a blood meal
Are difficult to detect because of their rapid movement
A sexually active adolescent male presents with the primary complaint of pubic and perianal pruritus. Careful examination reveals pubic or "crab" lice infestation. Of the following, the MOST characteristic feature of this infestation is that the lice:
Lay viable eggs that may hatch up to 7 days after being attached to a hair shaft
Only infest pubic and perianal regions
Rarely infest African-American patients
May survive for 36 hours without a blood meal
Are difficult to detect because of their rapid movement
You are evaluating a 6-hour-old male infant who was born after a term pregnancy and normal delivery and weighs 4 kg. The infant is comfortable but exhibits mild tachypnea, with a respiratory rate of 50 breaths/min. His heart rate is regular at 150 beats/min. His oxygen saturation is 60% in all extremities and does not increase significantly with the administration of oxygen by face mask. His lungs are clear, and there are no murmurs, gallops, or rub. You suspect transposition of the great arteries. Of the following, the BEST management strategy is
Intubation and mechanical ventilation with an Fio2 of 1.0
Increasing the right-to-left (pulmonary artery-to-aorta) shunt at the ductus arteriosus
Diuretic therapy intravenously for pulmonary edema
Increasing the left-to-right (aorta-to-pulmonary artery) shunt at the ductus arteriosus
Increasing the right-to-left shunt at the foramen ovale
You are evaluating a 6-hour-old male infant who was born after a term pregnancy and normal delivery and weighs 4 kg. The infant is comfortable but exhibits mild tachypnea, with a respiratory rate of 50 breaths/min. His heart rate is regular at 150 beats/min. His oxygen saturation is 60% in all extremities and does not increase significantly with the administration of oxygen by face mask. His lungs are clear, and there are no murmurs, gallops, or rub. You suspect transposition of the great arteries. Of the following, the BEST management strategy is
Intubation and mechanical ventilation with an Fio2 of 1.0
Increasing the right-to-left (pulmonary artery-to-aorta) shunt at the ductus arteriosus
Diuretic therapy intravenously for pulmonary edema
Increasing the left-to-right (aorta-to-pulmonary artery) shunt at the ductus arteriosus
Increasing the right-to-left shunt at the foramen ovale
A 6-year-old African-American child is brought in by his father for complaints of easy fatigability and pallor. These symptoms occurred after the son was treated with "some medication" for a recent diarrhea. Physical examination is normal except for pallor and multiple petechiae. Laboratory values are as follows: Hb 8.0 g/dL, WBC 12,000/mm3, Platelets 50,000/mm3, Blood glucose 118 mg/dL, Serum Na 135 mEq/L, Serum K 5.3 mEq/L, Chloride 110 mEq/L, Bicarbonate 18 mEq/L, BUN 38 mg/dL, Serum creatinine 2.5 mg/dL, Total bilirubin 3 mg/dL, Direct bilirubin 0.5 mg/dL, PT 12 seconds, APTT 30 seconds, LDH 900 IU/L, Reticulocyte count 6%. A peripheral blood smear reveals giant platelets and multiple schistocytes. What is the most likely underlying pathophysiology for this boy's pallor?
Folate deficiency
Microangiopathic hemolytic anemia
Thalassemia
Sickle cell anemia
Vitamin B12 deficiency
A 6-year-old African-American child is brought in by his father for complaints of easy fatigability and pallor. These symptoms occurred after the son was treated with "some medication" for a recent diarrhea. Physical examination is normal except for pallor and multiple petechiae. Laboratory values are as follows: Hb 8.0 g/dL, WBC 12,000/mm3, Platelets 50,000/mm3, Blood glucose 118 mg/dL, Serum Na 135 mEq/L, Serum K 5.3 mEq/L, Chloride 110 mEq/L, Bicarbonate 18 mEq/L, BUN 38 mg/dL, Serum creatinine 2.5 mg/dL, Total bilirubin 3 mg/dL, Direct bilirubin 0.5 mg/dL, PT 12 seconds, APTT 30 seconds, LDH 900 IU/L, Reticulocyte count 6%. A peripheral blood smear reveals giant platelets and multiple schistocytes. What is the most likely underlying pathophysiology for this boy's pallor?
Folate deficiency
Microangiopathic hemolytic anemia
Thalassemia
Sickle cell anemia
Vitamin B12 deficiency
A 5-month-old boy is brought in for a routine check-up. He was born at 37 weeks' gestation and has had persistent wheezing since shortly after birth despite inhaled bronchodilator and oral corticosteroid therapy. His diet consists of 32 ounces of iron-fortified cow's milk-based formula daily. On physical examination, the child appears well-nourished and happy. You note moderate relief of his wheezing with neck extension. Which of the following is the most likely mechanism of this infant's wheezing?
Chronic upper respiratory tract infection
Aspiration of a foreign body
Compression of the airway by a vascular ring
Allergic reaction to cow's milk
Asthma
A 5-month-old boy is brought in for a routine check-up. He was born at 37 weeks' gestation and has had persistent wheezing since shortly after birth despite inhaled bronchodilator and oral corticosteroid therapy. His diet consists of 32 ounces of iron-fortified cow's milk-based formula daily. On physical examination, the child appears well-nourished and happy. You note moderate relief of his wheezing with neck extension. Which of the following is the most likely mechanism of this infant's wheezing?
Chronic upper respiratory tract infection
Aspiration of a foreign body
Compression of the airway by a vascular ring
Allergic reaction to cow's milk
Asthma
A 22-year-old Caucasian female who has received no prenatal care experiences a stillbirth. This is her first pregnancy. The baby has multiple fractures, blue sclerae and short, bent extremities. Her past medical history is significant for a seizure disorder. She has been taking phenytoin regularly and had no seizure episodes during the pregnancy. She admits to eating poorly and occasionally drinking alcohol during the first trimester. She lives with her boyfriend who abuses her physically. She recalls several episodes of abuse during the pregnancy. Which of the following is most likely responsible for fetal abnormalities?
Alcohol abuse
Prenatal abuse
Collagen synthesis defect
Folic acid deficiency
Phenytoin use
A 22-year-old Caucasian female who has received no prenatal care experiences a stillbirth. This is her first pregnancy. The baby has multiple fractures, blue sclerae and short, bent extremities. Her past medical history is significant for a seizure disorder. She has been taking phenytoin regularly and had no seizure episodes during the pregnancy. She admits to eating poorly and occasionally drinking alcohol during the first trimester. She lives with her boyfriend who abuses her physically. She recalls several episodes of abuse during the pregnancy. Which of the following is most likely responsible for fetal abnormalities?
Alcohol abuse
Prenatal abuse
Collagen synthesis defect
Folic acid deficiency
Phenytoin use
A 3-year-old boy who was involved in a motor vehicle crash sustained a significant head injury and had a Glasgow Coma Scale score of 8 on arrival in the emergency department. An endotracheal tube was placed shortly after his arrival, and the respiratory therapist is providing ventilation at 12 breaths/min with 100% oxygen via a bag-valve mask until a ventilator can be brought to the emergency department. Ten minutes later, the child becomes more restless and agitated. His heart rate has increased from an initial 110 beats/min to about 150 beats/min, and he appears flushed. The monitor indicates that his oxygen saturation is 96%. Of the following, a TRUE statement about this child's ventilatory status is that
An arterial blood gas determination likely would reveal a pH of approximately 7.45
The oxygen saturation of 96% indicates that he is being ventilated adequately
A patient who has acute carbon dioxide retention due to hypoventilation still can have nearnormal blood oxygen saturation
His agitation is not related to his ventilatory status; it is due to tracheal irritation from the endotracheal tube
His agitation is due to relative hypoxemia
A 3-year-old boy who was involved in a motor vehicle crash sustained a significant head injury and had a Glasgow Coma Scale score of 8 on arrival in the emergency department. An endotracheal tube was placed shortly after his arrival, and the respiratory therapist is providing ventilation at 12 breaths/min with 100% oxygen via a bag-valve mask until a ventilator can be brought to the emergency department. Ten minutes later, the child becomes more restless and agitated. His heart rate has increased from an initial 110 beats/min to about 150 beats/min, and he appears flushed. The monitor indicates that his oxygen saturation is 96%. Of the following, a TRUE statement about this child's ventilatory status is that
An arterial blood gas determination likely would reveal a pH of approximately 7.45
The oxygen saturation of 96% indicates that he is being ventilated adequately
A patient who has acute carbon dioxide retention due to hypoventilation still can have nearnormal blood oxygen saturation
His agitation is not related to his ventilatory status; it is due to tracheal irritation from the endotracheal tube
His agitation is due to relative hypoxemia
A 7-year-old boy is referred for genetic testing because his father was diagnosed with medullary cancer of the thyroid. The father underwent a total thyroidectomy, and in the preoperative workup it was determined that he also had a pheochromocytoma, and that tumor was removed also. The father did not have parathyroid hyperplasia at the time, his phenotype was normal, and his final diagnosis was MEN-2A. The child is tested and found to have RET mutations in the peripheral white blood cells. The child has normal phenotype, normal levels of calcitonin, normal levels of catecholamines, metanephrines, and VMA, and normal levels of calcium and parathyroid hormone. Which of the following is the most appropriate management?
Bilateral adrenalectomies
Total thyroidectomy
Parathyroid surgical exploration
Continued observation
MRI of the pituitary
A 7-year-old boy is referred for genetic testing because his father was diagnosed with medullary cancer of the thyroid. The father underwent a total thyroidectomy, and in the preoperative workup it was determined that he also had a pheochromocytoma, and that tumor was removed also. The father did not have parathyroid hyperplasia at the time, his phenotype was normal, and his final diagnosis was MEN-2A. The child is tested and found to have RET mutations in the peripheral white blood cells. The child has normal phenotype, normal levels of calcitonin, normal levels of catecholamines, metanephrines, and VMA, and normal levels of calcium and parathyroid hormone. Which of the following is the most appropriate management?
Bilateral adrenalectomies
Total thyroidectomy
Parathyroid surgical exploration
Continued observation
MRI of the pituitary
{"name":"Pedia 2017 2018", "url":"https://www.supersurvey.com/QPREVIEW","txt":"A 3-day-old, full-term baby boy is brought into the emergency department because of feeding intolerance and bilious vomiting. X-rays films show multiple dilated loops of small bowel and a \"ground glass\" appearance in the lower abdomen. The mother has cystic fibrosis. Which of the following diagnostic tests would also have therapeutic value?, A 3-year-old boy is brought to the office by his Caucasian mother because his speech is difficult to understand. He is a very slow learner, is unusually calm, stays to himself, doesn't hug his parents, prefers to play by himself, speaks in mumbles, and repetitively tries to make towers with cubes. He becomes very aggressive if he is stopped from his activities. He was born at term from an uncomplicated pregnancy and delivery, and his physical growth has been normal. His brother used to be aggressive as a child, and was diagnosed with attention deficit hyperactivity disorder. In the office, the patient is sitting quietly and trying to make towers with cubes. He seems to be oblivious of his environment. On calling his name thrice, he turns towards you once and then resumes playing with the cubes. What do you tell his mother?, The parents of a 2-month-old baby boy are concerned about his risk of coronary artery disease because of the recent death of his 40- year-old maternal uncle from a myocardial infarction. Which of the following is the most appropriate management in this situation?","img":"https://www.quiz-maker.com/3012/CDN/92-4502225/screenshot-2023-08-24-221443.png?sz=1200-00000000001001808602"}